Gastroenterology is the branch of medicine focused on the digestive system and its disorders. The digestive system consists of the gastrointestinal tract, sometimes referred to as the GI tract, which includes the esophagus, stomach, small intestine and large intestine as well as the accessory organs of digestion which include the pancreas, gallbladder, and liver. The digestive system functions to move material through the GI tract via peristalsis, break down that material via digestion, absorb nutrients for use throughout the body, and remove waste from the body via defecation. Physicians who specialize in the medical specialty of gastroenterology are called gastroenterologists or sometimes GI doctors. Some of the most common conditions managed by gastroenterologists include gastroesophageal reflux disease, gastrointestinal bleeding, irritable bowel syndrome, inflammatory bowel disease (IBD) which includes Crohn's disease and ulcerative colitis, peptic ulcer disease, gallbladder and biliary tract disease, hepatitis, pancreatitis, colitis, colon polyps and cancer, nutritional problems, and many more.

Haematochezia is the passage of fresh blood through the anus path, usually in or with stools. The term is from Greek αἷμα ("blood") and χέζειν. Hematochezia is commonly associated with lower gastrointestinal bleeding, but may also occur from a brisk upper gastrointestinal bleed. The difference between hematochezia and rectorrhagia is that, in the latter, rectal bleeding is not associated with defecation; instead, it is associated with expulsion of fresh bright red blood without stools. The phrase bright red blood per rectum is associated with hematochezia and rectorrhagia.

Upper gastrointestinal bleeding is gastrointestinal bleeding in the upper gastrointestinal tract, commonly defined as bleeding arising from the esophagus, stomach, or duodenum. Blood may be observed in vomit or in altered form as black stool. Depending on the amount of the blood loss, symptoms may include shock.
Coffee ground vomitus refers to a particular appearance of vomit. Within organic heme molecules of red blood cells is the element iron, which oxidizes following exposure to gastric acid. This reaction causes the vomitus to look like ground coffee.

Heyde's syndrome is a syndrome of gastrointestinal bleeding from angiodysplasia in the presence of aortic stenosis.

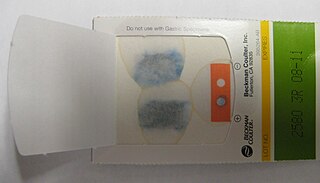
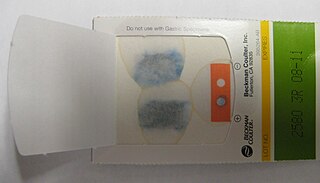
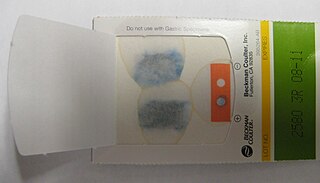
Fecal occult blood (FOB) refers to blood in the feces that is not visibly apparent. A fecal occult blood test (FOBT) checks for hidden (occult) blood in the stool (feces).

Esophagogastroduodenoscopy (EGD) or oesophagogastroduodenoscopy (OGD), also called by various other names, is a diagnostic endoscopic procedure that visualizes the upper part of the gastrointestinal tract down to the duodenum. It is considered a minimally invasive procedure since it does not require an incision into one of the major body cavities and does not require any significant recovery after the procedure. However, a sore throat is common.
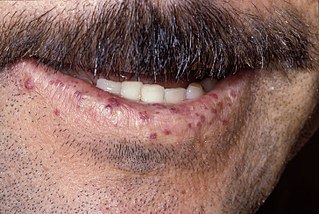
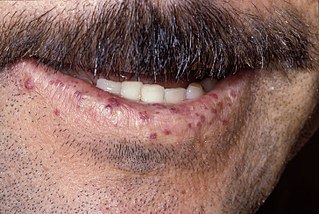
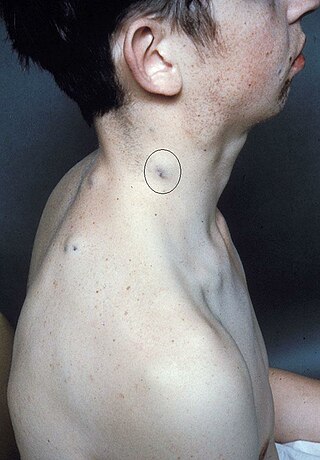
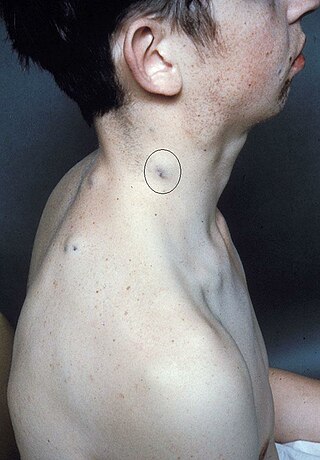
Hereditary hemorrhagic telangiectasia (HHT), also known as Osler–Weber–Rendu disease and Osler–Weber–Rendu syndrome, is a rare autosomal dominant genetic disorder that leads to abnormal blood vessel formation in the skin, mucous membranes, and often in organs such as the lungs, liver, and brain.

Dieulafoy's lesion is a medical condition characterized by a large tortuous artery most commonly in the stomach wall (submucosal) that erodes and bleeds. It can present in any part of the gastrointestinal tract. It can cause gastric hemorrhage but is relatively uncommon. It is thought to cause less than 5% of all gastrointestinal bleeds in adults. It was named after French surgeon Paul Georges Dieulafoy, who described this condition in his paper "Exulceratio simplex: Leçons 1-3" in 1898. It is also called "caliber-persistent artery" or "aneurysm" of gastric vessels. However, unlike most other aneurysms, these are thought to be developmental malformations rather than degenerative changes.
Gastrointestinal bleeding, also called gastrointestinal hemorrhage (GIB), is all forms of bleeding in the gastrointestinal tract, from the mouth to the rectum. When there is significant blood loss over a short time, symptoms may include vomiting red blood, vomiting black blood, bloody stool, or black stool. Small amounts of bleeding over a long time may cause iron-deficiency anemia resulting in feeling tired or heart-related chest pain. Other symptoms may include abdominal pain, shortness of breath, pale skin, or passing out. Sometimes in those with small amounts of bleeding no symptoms may be present.

Blood in stool or rectal bleeding looks different depending on how early it enters the digestive tract—and thus how much digestive action it has been exposed to—and how much there is. The term can refer either to melena, with a black appearance, typically originating from upper gastrointestinal bleeding; or to hematochezia, with a red color, typically originating from lower gastrointestinal bleeding. Evaluation of the blood found in stool depends on its characteristics, in terms of color, quantity and other features, which can point to its source, however, more serious conditions can present with a mixed picture, or with the form of bleeding that is found in another section of the tract. The term "blood in stool" is usually only used to describe visible blood, and not fecal occult blood, which is found only after physical examination and chemical laboratory testing.
Lower gastrointestinal bleeding, commonly abbreviated LGIB, is any form of gastrointestinal bleeding in the lower gastrointestinal tract. LGIB is a common reason for seeking medical attention at a hospital's emergency department. LGIB accounts for 30–40% of all gastrointestinal bleeding and is less common than upper gastrointestinal bleeding (UGIB). It is estimated that UGIB accounts for 100–200 per 100,000 cases versus 20–27 per 100,000 cases for LGIB. Approximately 85% of lower gastrointestinal bleeding involves the colon, 10% are from bleeds that are actually upper gastrointestinal bleeds, and 3–5% involve the small intestine.

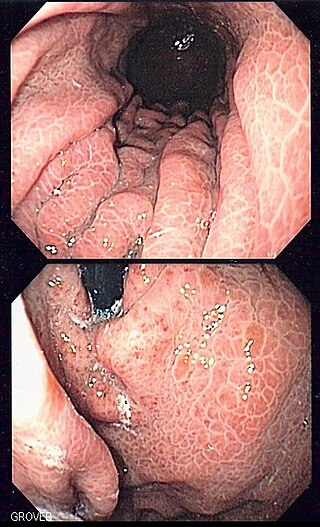
Gastric antral vascular ectasia (GAVE) is an uncommon cause of chronic gastrointestinal bleeding or iron deficiency anemia. The condition is associated with dilated small blood vessels in the pyloric antrum, which is a distal part of the stomach. The dilated vessels result in intestinal bleeding. It is also called watermelon stomach because streaky long red areas that are present in the stomach may resemble the markings on watermelon.

Ischemic colitis is a medical condition in which inflammation and injury of the large intestine result from inadequate blood supply. Although uncommon in the general population, ischemic colitis occurs with greater frequency in the elderly, and is the most common form of bowel ischemia. Causes of the reduced blood flow can include changes in the systemic circulation or local factors such as constriction of blood vessels or a blood clot. In most cases, no specific cause can be identified.

Double-balloon enteroscopy, also known as push-and-pull enteroscopy, is an endoscopic technique for visualization of the small bowel. It was developed by Hironori Yamamoto in 2001. It is novel in the field of diagnostic gastroenterology as it is the first endoscopic technique that allows for the entire gastrointestinal tract to be visualized in real time.

Hemosuccus pancreaticus is a rare cause of hemorrhage in the gastrointestinal tract. It is caused by a bleeding source in the pancreas, pancreatic duct, or structures adjacent to the pancreas, such as the splenic artery, that bleed into the pancreatic duct, which is connected with the bowel at the duodenum, the first part of the small intestine. Patients with hemosuccus may develop symptoms of gastrointestinal hemorrhage, such as blood in the stools, maroon stools, or melena, which is a dark, tarry stool caused by digestion of red blood cells. They may also develop abdominal pain. It is associated with pancreatitis, pancreatic cancer and aneurysms of the splenic artery. Hemosuccus may be identified with endoscopy (esophagogastroduodenoscopy), where fresh blood may be seen from the pancreatic duct. Alternatively, angiography may be used to inject the celiac axis to determine the blood vessel that is bleeding. This may also be used to treat hemosuccus, as embolization of the end vessel may terminate the hemorrhage. However, a distal pancreatectomy—surgery to remove of the tail of the pancreas—may be required to stop the hemorrhage.
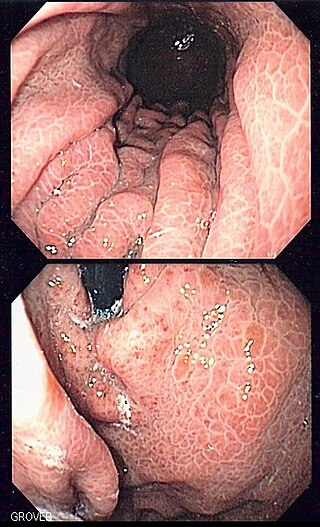
Portal hypertensive gastropathy refers to changes in the mucosa of the stomach in patients with portal hypertension; by far the most common cause of this is cirrhosis of the liver. These changes in the mucosa include friability of the mucosa and the presence of ectatic blood vessels at the surface. Patients with portal hypertensive gastropathy may experience bleeding from the stomach, which may uncommonly manifest itself in vomiting blood or melena; however, portal hypertension may cause several other more common sources of upper gastrointestinal bleeding, such as esophageal varices and gastric varices. On endoscopic evaluation of the stomach, this condition shows a characteristic mosaic or "snake-skin" appearance to the mucosa of the stomach.

A colorectal polyp is a polyp occurring on the lining of the colon or rectum. Untreated colorectal polyps can develop into colorectal cancer.
A Cameron lesion is a linear erosion or ulceration of the mucosal folds lining the stomach where it is constricted by the thoracic diaphragm in persons with large hiatal hernias. The lesions may cause chronic blood loss resulting in iron deficiency anemia; less often they cause acute bleeding.
Blue rubber bleb nevus syndrome is a rare disorder that consists mainly of abnormal blood vessels affecting the skin or internal organs – usually the gastrointestinal tract. The disease is characterized by the presence of fluid-filled blisters (blebs) as visible, circumscribed, chronic lesions (nevi).