Trichuris trichiura, Trichocephalus trichiuris or whipworm, is a parasitic roundworm that causes trichuriasis when it infects a human large intestine. It is commonly known as the whipworm which refers to the shape of the worm; it looks like a whip with wider "handles" at the posterior end.

Crohn's disease is a type of inflammatory bowel disease (IBD) that may affect any segment of the gastrointestinal tract. Symptoms often include abdominal pain, diarrhea, fever, abdominal distension, and weight loss. Complications outside of the gastrointestinal tract may include anemia, skin rashes, arthritis, inflammation of the eye, and fatigue. The skin rashes may be due to infections as well as pyoderma gangrenosum or erythema nodosum. Bowel obstruction may occur as a complication of chronic inflammation, and those with the disease are at greater risk of colon cancer and small bowel cancer.

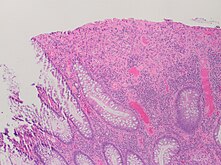
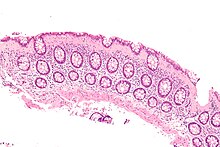
Ulcerative colitis (UC) is one of the two types of inflammatory bowel disease (IBD), with the other type being Crohn's disease. It is a long-term condition that results in inflammation and ulcers of the colon and rectum. The primary symptoms of active disease are abdominal pain and diarrhea mixed with blood (hematochezia). Weight loss, fever, and anemia may also occur. Often, symptoms come on slowly and can range from mild to severe. Symptoms typically occur intermittently with periods of no symptoms between flares. Complications may include abnormal dilation of the colon (megacolon), inflammation of the eye, joints, or liver, and colon cancer.

Inflammatory bowel disease (IBD) is a group of inflammatory conditions of the colon and small intestine, with Crohn's disease and ulcerative colitis (UC) being the principal types. Crohn's disease affects the small intestine and large intestine, as well as the mouth, esophagus, stomach and the anus, whereas UC primarily affects the colon and the rectum.
Toxic megacolon is an acute form of colonic distension. It is characterized by a very dilated colon (megacolon), accompanied by abdominal distension (bloating), and sometimes fever, abdominal pain, or shock.
In medicine, the ileal pouch–anal anastomosis (IPAA), also known as restorative proctocolectomy (RPC), ileal-anal reservoir (IAR), an ileo-anal pouch, ileal-anal pullthrough, or sometimes referred to as a J-pouch, S-pouch, W-pouch, or a pelvic pouch, is an anastomosis of a reservoir pouch made from ileum to the anus, bypassing the former site of the colon in cases where the colon and rectum have been removed. The pouch retains and restores functionality of the anus, with stools passed under voluntary control of the person, preventing fecal incontinence and serving as an alternative to a total proctocolectomy with ileostomy.

Megacolon is an abnormal dilation of the colon. This leads to hypertrophy of the colon. The dilation is often accompanied by a paralysis of the peristaltic movements of the bowel. In more extreme cases, the feces consolidate into hard masses inside the colon, called fecalomas, which can require surgery to be removed.

Helminthic therapy, an experimental type of immunotherapy, is the treatment of autoimmune diseases and immune disorders by means of deliberate infestation with a helminth or with the eggs of a helminth. Helminths are parasitic worms such as hookworms, whipworms, and threadworms that have evolved to live within a host organism on which they rely for nutrients. These worms are members of two phyla: nematodes, which are primarily used in human helminthic therapy, and flat worms (trematodes).

Blood in stool or rectal bleeding looks different depending on how early it enters the digestive tract—and thus how much digestive action it has been exposed to—and how much there is. The term can refer either to melena, with a black appearance, typically originating from upper gastrointestinal bleeding; or to hematochezia, with a red color, typically originating from lower gastrointestinal bleeding. Evaluation of the blood found in stool depends on its characteristics, in terms of color, quantity and other features, which can point to its source, however, more serious conditions can present with a mixed picture, or with the form of bleeding that is found in another section of the tract. The term "blood in stool" is usually only used to describe visible blood, and not fecal occult blood, which is found only after physical examination and chemical laboratory testing.
Pouchitis is an umbrella term for inflammation of the ileal pouch, an artificial rectum surgically created out of ileum in patients who have undergone a proctocolectomy or total colectomy. The ileal pouch-anal anastomosis is created in the management of patients with ulcerative colitis, indeterminate colitis, familial adenomatous polyposis, cancer, or rarely, other colitides.

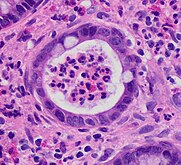
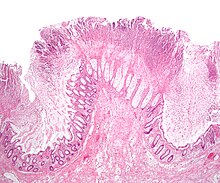
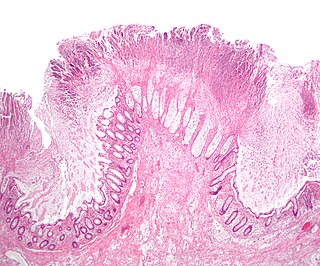
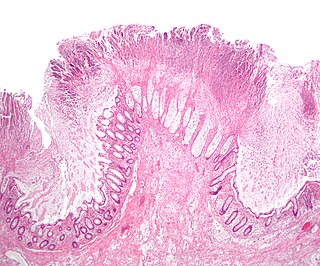
Microscopic colitis refers to two related medical conditions which cause diarrhea: collagenous colitis and lymphocytic colitis. Both conditions are characterized by the presence of chronic non-bloody watery diarrhea, normal appearances on colonoscopy and characteristic histopathology findings of inflammatory cells.

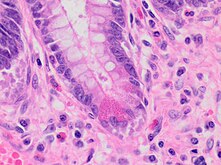
Collagenous colitis is an inflammatory condition of the colon. Together with the related condition lymphocytic colitis, it is a subtype of microscopic colitis, which is characterized by inflammation that specifically affects the colon, and a clinical presentation that involves watery diarrhea but a lack of rectal bleeding. Microscopic colitis does not usually cause macroscopic changes to the colon that allow a visual diagnosis during colonoscopy, instead causing microscopic changes that can be detected through histopathological examination of colonic biopsies. The nature of these microscopic changes is what differentiates collagenous from lymphocytic colitis, with the characteristic finding in collagenous colitis being depositions of collagen in the connective tissue between the colonic glands. Collagenous colitis, and microscopic colitis as a whole, is sometimes considered to be an inflammatory bowel disease (IBD) along with Crohn's disease and ulcerative colitis. However, little is known about the etiology of microscopic colitis, and so the degree of similarity to the inflammatory bowel diseases is uncertain.
Management of Crohn's disease involves first treating the acute symptoms of the disease, then maintaining remission. Since Crohn's disease is an immune system condition, it cannot be cured by medication or surgery. Treatment initially involves the use of medications to eliminate infections and reduce inflammation. Surgery may be required for complications such as obstructions, fistulae, abscesses, or if the disease does not respond to drugs within a reasonable time. However, surgery cannot cure Crohn's disease. It involves removing the diseased part of the intestine and rejoining the healthy ends, but the disease tends to recur after surgery.
Management of ulcerative colitis involves first treating the acute symptoms of the disease, then maintaining remission. Ulcerative colitis is a form of colitis, a disease of the intestine, specifically the large intestine or colon, that includes characteristic ulcers, or open sores, in the colon. The main symptom of active disease is usually diarrhea mixed with blood, of gradual onset which often leads to anaemia. Ulcerative colitis is, however, a systemic disease that affects many parts of the body outside the intestine.
Dysbiosis is characterized by a disruption to the microbiome resulting in an imbalance in the microbiota, changes in their functional composition and metabolic activities, or a shift in their local distribution. For example, a part of the human microbiota such as the skin flora, gut flora, or vaginal flora, can become deranged, with normally dominating species underrepresented and normally outcompeted or contained species increasing to fill the void. Similar to the human gut microbiome, diverse microbes colonize the plant rhizosphere, and dysbiosis in the rhizosphere, can negatively impact plant health. Dysbiosis is most commonly reported as a condition in the gastrointestinal tract or plant rhizosphere.

Biological therapy, the use of medications called biopharmaceuticals or biologics that are tailored to specifically target an immune or genetic mediator of disease, plays a major role in the treatment of inflammatory bowel disease. Even for diseases of unknown cause, molecules that are involved in the disease process have been identified, and can be targeted for biological therapy. Many of these molecules, which are mainly cytokines, are directly involved in the immune system. Biological therapy has found a niche in the management of cancer, autoimmune diseases, and diseases of unknown cause that result in symptoms due to immune related mechanisms.

Pancolitis, in its most general sense, refers to inflammation of the entire colon. This can be caused by a variety of things. Pancolitis or universal colitis is frequently used in a more specific fashion to denote a very severe form of ulcerative colitis. This form of ulcerative colitis is spread throughout the entire large intestine including the right colon, the left colon, the transverse colon, descending colon, and the rectum. A diagnosis can be made using a number of techniques but the most accurate method is direct visualization via a colonoscopy. Symptoms are similar to those of ulcerative colitis but more severe and affect the entire large intestine. Patients with ulcerative colitis generally exhibit symptoms including rectal bleeding as a result of ulcers, pain in the abdominal region, inflammation in varying degrees, and diarrhea. Pancolitis patients exhibit these symptoms and may also experience fatigue, fever, and night sweats. Due to the loss of function in the large intestine patients may lose large amounts of weight from being unable to procure nutrients from food. In other cases the blood loss from ulcers can result in anemia which can be treated with iron supplements. Additionally, due to the chronic nature of most cases of pancolitis, patients have a higher chance of developing colon cancer.

Enteropathic arthropathy commonly referred to as enteropathic arthritis, is a type of arthritis linked to Crohn's disease, ulcerative colitis, and chronic inflammatory bowel diseases.

Segmental colitis associated with diverticulosis (SCAD) is a condition characterized by localized inflammation in the colon, which spares the rectum and is associated with multiple sac-like protrusions or pouches in the wall of the colon (diverticulosis). Unlike diverticulitis, SCAD involves inflammation of the colon between diverticula, while sparing the diverticular orifices. SCAD may lead to abdominal pain, especially in the left lower quadrant, intermittent rectal bleeding and chronic diarrhea.
Shomron Ben-Horin is an Israeli physician, a co-founder & Chief Medical Officer of Evinature, and professor of medicine at the Tel-Aviv University.