Shoulder problems including pain, are one of the more common reasons for physician visits for musculoskeletal symptoms. The shoulder is the most movable joint in the body. However, it is an unstable joint because of the range of motion allowed. This instability increases the likelihood of joint injury, often leading to a degenerative process in which tissues break down and no longer function well.

A bone fracture is a medical condition in which there is a partial or complete break in the continuity of any bone in the body. In more severe cases, the bone may be broken into several fragments, known as a comminuted fracture. A bone fracture may be the result of high force impact or stress, or a minimal trauma injury as a result of certain medical conditions that weaken the bones, such as osteoporosis, osteopenia, bone cancer, or osteogenesis imperfecta, where the fracture is then properly termed a pathologic fracture.

A joint dislocation, also called luxation, occurs when there is an abnormal separation in the joint, where two or more bones meet. A partial dislocation is referred to as a subluxation. Dislocations are often caused by sudden trauma on the joint like an impact or fall. A joint dislocation can cause damage to the surrounding ligaments, tendons, muscles, and nerves. Dislocations can occur in any major joint or minor joint. The most common joint dislocation is a shoulder dislocation.

A distal radius fracture, also known as wrist fracture, is a break of the part of the radius bone which is close to the wrist. Symptoms include pain, bruising, and rapid-onset swelling. The ulna bone may also be broken.

A hip fracture is a break that occurs in the upper part of the femur, at the femoral neck or (rarely) the femoral head. Symptoms may include pain around the hip, particularly with movement, and shortening of the leg. Usually the person cannot walk.

An avulsion fracture is a bone fracture which occurs when a fragment of bone tears away from the main mass of bone as a result of physical trauma. This can occur at the ligament by the application of forces external to the body or at the tendon by a muscular contraction that is stronger than the forces holding the bone together. Generally muscular avulsion is prevented by the neurological limitations placed on muscle contractions. Highly trained athletes can overcome this neurological inhibition of strength and produce a much greater force output capable of breaking or avulsing a bone.

Nonunion is permanent failure of healing following a broken bone unless intervention is performed. A fracture with nonunion generally forms a structural resemblance to a fibrous joint, and is therefore often called a "false joint" or pseudoarthrosis. The diagnosis is generally made when there is no healing between two sets of medical imaging, such as X-ray or CT scan. This is generally after 6–8 months.

Flail chest is a life-threatening medical condition that occurs when a segment of the rib cage breaks due to trauma and becomes detached from the rest of the chest wall. Two of the symptoms of flail chest are chest pain and shortness of breath.

An ankle fracture is a break of one or more of the bones that make up the ankle joint. Symptoms may include pain, swelling, bruising, and an inability to walk on the injured leg. Complications may include an associated high ankle sprain, compartment syndrome, stiffness, malunion, and post-traumatic arthritis.

A patella fracture is a break of the kneecap. Symptoms include pain, swelling, and bruising to the front of the knee. A person may also be unable to walk. Complications may include injury to the tibia, femur, or knee ligaments.

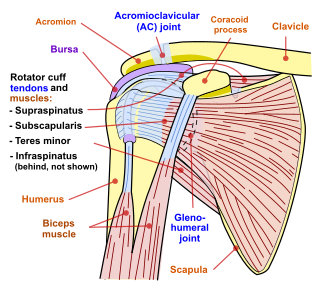
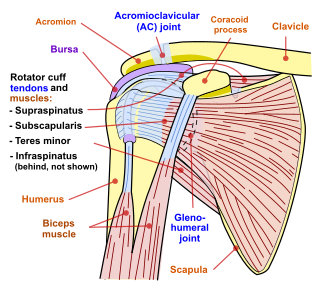
A separated shoulder, also known as acromioclavicular joint injury, is a common injury to the acromioclavicular joint. The AC joint is located at the outer end of the clavicle where it attaches to the acromion of the scapula. Symptoms include non-radiating pain which may make it difficult to move the shoulder. The presence of swelling or bruising and a deformity in the shoulder is also common depending on how severe the dislocation is.
Shoulder surgery is a means of treating injured shoulders. Many surgeries have been developed to repair the muscles, connective tissue, or damaged joints that can arise from traumatic or overuse injuries to the shoulder.

A scaphoid fracture is a break of the scaphoid bone in the wrist. Symptoms generally includes pain at the base of the thumb which is worse with use of the hand. The anatomic snuffbox is generally tender and swelling may occur. Complications may include nonunion of the fracture, avascular necrosis of the proximal part of the bone, and arthritis.

The Le Fortfractures are a pattern of midface fractures originally described by the French surgeon, René Le Fort, in the early 1900s. He described three distinct fracture patterns. Although not always applicable to modern-day facial fractures, the Le Fort type fracture classification is still utilized today by medical providers to aid in describing facial trauma for communication, documentation, and surgical planning. Several surgical techniques have been established for facial reconstruction following Le Fort fractures, including maxillomandibular fixation (MMF) and open reduction and internal fixation (ORIF). The main goal of any surgical intervention is to re-establish occlusion, or the alignment of upper and lower teeth, to ensure the patient is able to eat. Complications following Le Fort fractures rely on the anatomical structures affected by the inciding injury.

A humerus fracture is a break of the humerus bone in the upper arm. Symptoms may include pain, swelling, and bruising. There may be a decreased ability to move the arm and the person may present holding their elbow. Complications may include injury to an artery or nerve, and compartment syndrome.

Internal fixation is an operation in orthopedics that involves the surgical implementation of implants for the purpose of repairing a bone, a concept that dates to the mid-nineteenth century and was made applicable for routine treatment in the mid-twentieth century. An internal fixator may be made of stainless steel, titanium alloy, or cobalt-chrome alloy. or plastics.

A bimalleolar fracture is a fracture of the ankle that involves the lateral malleolus and the medial malleolus. Studies have shown that bimalleolar fractures are more common in women, people over 60 years of age, and patients with existing comorbidities.

A femoral fracture is a bone fracture that involves the femur. They are typically sustained in high-impact trauma, such as car crashes, due to the large amount of force needed to break the bone. Fractures of the diaphysis, or middle of the femur, are managed differently from those at the head, neck, and trochanter; those are conventionally called hip fractures. Thus, mentions of femoral fracture in medicine usually refer implicitly to femoral fractures at the shaft or distally.

Orthopedic surgery is the branch of surgery concerned with conditions involving the musculoskeletal system. Orthopedic surgeons use both surgical and nonsurgical means to treat musculoskeletal injuries, sports injuries, degenerative diseases, infections, bone tumours, and congenital limb deformities. Trauma surgery and traumatology is a sub-specialty dealing with the operative management of fractures, major trauma and the multiply-injured patient.

A proximal humerus fracture is a break of the upper part of the bone of the arm (humerus). Symptoms include pain, swelling, and a decreased ability to move the shoulder. Complications may include axillary nerve or axillary artery injury.