Cartilage is a resilient and smooth type of connective tissue. It is a semi-transparent and non-porous type of tissue. It is usually covered by a tough and fibrous membrane called perichondrium. In tetrapods, it covers and protects the ends of long bones at the joints as articular cartilage, and is a structural component of many body parts including the rib cage, the neck and the bronchial tubes, and the intervertebral discs. In other taxa, such as chondrichthyans, but also in cyclostomes, it may constitute a much greater proportion of the skeleton. It is not as hard and rigid as bone, but it is much stiffer and much less flexible than muscle. The matrix of cartilage is made up of glycosaminoglycans, proteoglycans, collagen fibers and, sometimes, elastin. It usually grows quicker than bone.

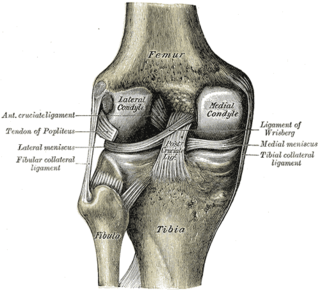
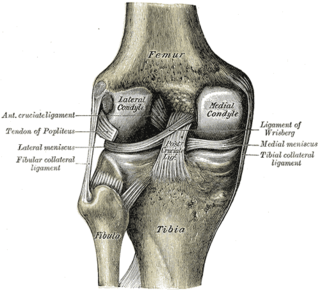
In humans and other primates, the knee joins the thigh with the leg and consists of two joints: one between the femur and tibia, and one between the femur and patella. It is the largest joint in the human body. The knee is a modified hinge joint, which permits flexion and extension as well as slight internal and external rotation. The knee is vulnerable to injury and to the development of osteoarthritis.

Osteoarthritis (OA) is a type of degenerative joint disease that results from breakdown of joint cartilage and underlying bone. It is believed to be the fourth leading cause of disability in the world, affecting 1 in 7 adults in the United States alone. The most common symptoms are joint pain and stiffness. Usually the symptoms progress slowly over years. Other symptoms may include joint swelling, decreased range of motion, and, when the back is affected, weakness or numbness of the arms and legs. The most commonly involved joints are the two near the ends of the fingers and the joint at the base of the thumbs, the knee and hip joints, and the joints of the neck and lower back. The symptoms can interfere with work and normal daily activities. Unlike some other types of arthritis, only the joints, not internal organs, are affected.
Chondropathy refers to a disease of the cartilage. It is frequently divided into 5 grades, with 0-2 defined as normal and 3-4 defined as diseased.

Osteochondritis dissecans is a joint disorder primarily of the subchondral bone in which cracks form in the articular cartilage and the underlying subchondral bone. OCD usually causes pain during and after sports. In later stages of the disorder there will be swelling of the affected joint which catches and locks during movement. Physical examination in the early stages does only show pain as symptom, in later stages there could be an effusion, tenderness, and a crackling sound with joint movement.

Chondrogenesis is the process by which cartilage is developed.
Articular cartilage, most notably that which is found in the knee joint, is generally characterized by very low friction, high wear resistance, and poor regenerative qualities. It is responsible for much of the compressive resistance and load bearing qualities of the knee joint and, without it, walking is painful to impossible. Osteoarthritis is a common condition of cartilage failure that can lead to limited range of motion, bone damage and invariably, pain. Due to a combination of acute stress and chronic fatigue, osteoarthritis directly manifests itself in a wearing away of the articular surface and, in extreme cases, bone can be exposed in the joint. Some additional examples of cartilage failure mechanisms include cellular matrix linkage rupture, chondrocyte protein synthesis inhibition, and chondrocyte apoptosis. There are several different repair options available for cartilage damage or failure.

The triangular fibrocartilage complex (TFCC) is formed by the triangular fibrocartilage discus (TFC), the radioulnar ligaments (RULs) and the ulnocarpal ligaments (UCLs).
Microfracture surgery is an articular cartilage repair surgical technique that works by creating tiny fractures in the underlying bone. This causes new cartilage to develop from a so-called super-clot.

A tear of a meniscus is a rupturing of one or more of the fibrocartilage strips in the knee called menisci. When doctors and patients refer to "torn cartilage" in the knee, they actually may be referring to an injury to a meniscus at the top of one of the tibiae. Menisci can be torn during innocuous activities such as walking or squatting. They can also be torn by traumatic force encountered in sports or other forms of physical exertion. The traumatic action is most often a twisting movement at the knee while the leg is bent. In older adults, the meniscus can be damaged following prolonged 'wear and tear'. Especially acute injuries can lead to displaced tears which can cause mechanical symptoms such as clicking, catching, or locking during motion of the joint. The joint will be in pain when in use, but when there is no load, the pain goes away.
Articular cartilage repair treatment involves the repair of the surface of the articular joint's hyaline cartilage, though these solutions do not perfectly restore the articular cartilage. These treatments have been shown to have positive results for patients who have articular cartilage damage. They can provide some measure of pain relief, while slowing down the accumulation of damage, or delaying the need for joint replacement surgery.
Autologous chondrocyte implantation is a biomedical treatment that repairs damages in articular cartilage. ACI provides pain relief while at the same time slowing down the progression or considerably delaying partial or total joint replacement surgery. The goal of ACI is to allow people suffering from articular cartilage damage to return to their old lifestyle; regaining mobility, going back to work and even practicing sports again.
Mesenchymal stem cells (MSCs) are multipotent cells found in multiple human adult tissues, including bone marrow, synovial tissues, and adipose tissues. Since they are derived from the mesoderm, they have been shown to differentiate into bone, cartilage, muscle, and adipose tissue. MSCs from embryonic sources have shown promise scientifically while creating significant controversy. As a result, many researchers have focused on adult stem cells, or stem cells isolated from adult humans that can be transplanted into damaged tissue.
Autologous matrix-induced chondrogenesis (AMIC) is a treatment for articular cartilage damage. It combines microfracture surgery with the application of a bi-layer collagen I/III membrane. There is tentative short to medium term benefits as of 2017.
Cartilage repair techniques are the current focus of large amounts of research. Many different strategies have been proposed as solutions for cartilage defects. Surgical techniques currently being studied include:
Gene therapy for osteoarthritis is the application of gene therapy to treat osteoarthritis (OA). Unlike pharmacological treatments which are administered locally or systemically as a series of interventions, gene therapy aims to establish sustained therapeutic effect after a single, local injection.
The treatment of equine lameness is a complex subject. Lameness in horses has a variety of causes, and treatment must be tailored to the type and degree of injury, as well as the financial capabilities of the owner. Treatment may be applied locally, systemically, or intralesionally, and the strategy for treatment may change as healing progresses. The end goal is to reduce the pain and inflammation associated with injury, to encourage the injured tissue to heal with normal structure and function, and to ultimately return the horse to the highest level of performance possible following recovery.

Pain in the hip is the experience of pain in the muscles or joints in the hip/ pelvic region, a condition commonly arising from any of a number of factors. Sometimes it is closely associated with lower back pain.
Artificial cartilage is a synthetic material made of hydrogels or polymers that aims to mimic the functional properties of natural cartilage in the human body. Tissue engineering principles are used in order to create a non-degradable and biocompatible material that can replace cartilage. While creating a useful synthetic cartilage material, certain challenges need to be overcome. First, cartilage is an avascular structure in the body and therefore does not repair itself. This creates issues in regeneration of the tissue. Synthetic cartilage also needs to be stably attached to its underlying surface i.e. the bone. Lastly, in the case of creating synthetic cartilage to be used in joint spaces, high mechanical strength under compression needs to be an intrinsic property of the material.
Spheroids of human autologous matrix-associated chondrocytes, sold under the brand name Spherox, is a medication used to repair defects to the cartilage in the knee in adults who are experiencing knee pain and problems moving the knee. It is used where the affected area is no larger than 10 cm2 (1.6 sq in).