A cataract is a cloudy area in the lens of the eye that leads to a decrease in vision. Cataracts often develop slowly and can affect one or both eyes. Symptoms may include faded colors, blurry or double vision, halos around light, trouble with bright lights, and trouble seeing at night. This may result in trouble driving, reading, or recognizing faces. Poor vision caused by cataracts may also result in an increased risk of falling and depression. Cataracts cause half of all cases of blindness and 33% of visual impairment worldwide.

Vitrectomy is a surgery to remove some or all of the vitreous humor from the eye.

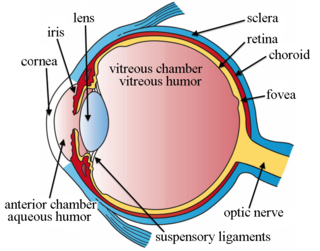
Macular edema occurs when fluid and protein deposits collect on or under the macula of the eye and causes it to thicken and swell (edema). The swelling may distort a person's central vision, because the macula holds tightly packed cones that provide sharp, clear, central vision to enable a person to see detail, form, and color that is directly in the centre of the field of view.

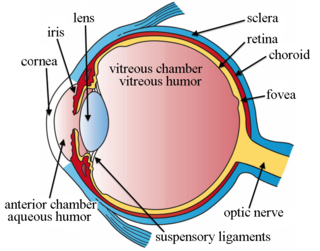
Uveitis is the inflammation of the uvea, the pigmented layer that lies between the inner retina and the outer fibrous layer composed of the sclera and cornea. The uvea consists of the middle layer of pigmented vascular structures of the eye and includes the iris, ciliary body, and choroid. Uveitis is described anatomically, by the part of the eye affected, as anterior, intermediate or posterior, from front to back. In the panuveitic form, all parts are involved. The most common form is the anterior one. Symptoms include pain, floaters and blurred vision, and clinical examination may show redness and an irregular pupil, while ophthalmic examination shows dilated ciliary blood vessels and the presence of cells in the anterior chamber. Uveitis may arise spontaneously and associated with some genetic factors, or be associated with a wide range of conditions including autoimmune disease and infections. While the eye is a relatively protected environment, its immune mechanisms may be overcome resulting in inflammation and tissue destruction associated with T-cell activation. The incidence is approximately 1:4500, most commonly between the ages of 20–60.

Cataract surgery, also called lens replacement surgery, is the removal of the natural lens of the eye that has developed an opacification, which is referred to as a cataract, and its replacement with an intraocular lens. Metabolic changes of the crystalline lens fibers over time lead to the development of the cataract, causing impairment or loss of vision. Some infants are born with congenital cataracts, and certain environmental factors may also lead to cataract formation. Early symptoms may include strong glare from lights and small light sources at night, and reduced acuity at low light levels.

Cytomegalovirus retinitis, also known as CMV retinitis, is an inflammation of the retina of the eye that can lead to blindness. Caused by human cytomegalovirus, it occurs predominantly in people whose immune system has been compromised, 15-40% of those with AIDS.
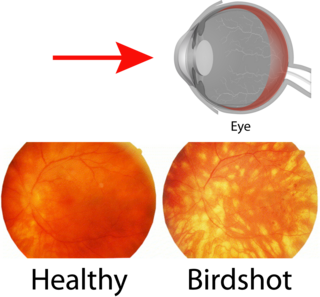
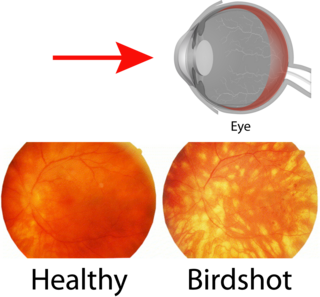
Birdshot chorioretinopathy, now commonly named birdshot uveitis or HLA-A29 uveitis, is a rare form of bilateral posterior uveitis affecting both eyes. It causes severe, progressive inflammation of both the choroid and retina.
Eales disease is a type of obliterative vasculopathy, also known as angiopathia retinae juvenilis, periphlebitis retinae, primary perivasculitis of the retina. It was first described by the British ophthalmologist Henry Eales (1852–1913) in 1880 and is a rare ocular disease characterized by inflammation and possible blockage of retinal blood vessels, abnormal growth of new blood vessels (neovascularization), and recurrent retinal and vitreal hemorrhages. This disease is identified by its three characteristic steps: vasculitis, occlusion, and retinal neovascularization, leading to recurrent vitreous hemorrhages and vision loss. Eales Disease with a characteristic clinical picture, fluorescein angiographic finding, and natural course is considered a specific disease entity. The exact cause of this disease is unknown but it appears to affect individuals that are from Asian subcontinents. This disease tends to begin between the ages of 20-30 years and begins with unilateral peripheral retinal perivasculitis and peripheral retinal capillary non-perfusion. These are not normally recognized until the inflammation results in vitreous hemorrhage. This disease has been found to affect the second eye 50-90% of the time so there is a large chance that both eyes will begin to show signs of the disease.

Epiretinal membrane or macular pucker is a disease of the eye in response to changes in the vitreous humor or more rarely, diabetes. Sometimes, as a result of immune system response to protect the retina, cells converge in the macular area as the vitreous ages and pulls away in posterior vitreous detachment (PVD). PVD can create minor damage to the retina, stimulating exudate, inflammation, and leucocyte response. These cells can form a transparent layer gradually and, like all scar tissue, tighten to create tension on the retina which may bulge and pucker, or even cause swelling or macular edema. Often this results in distortions of vision that are clearly visible as bowing and blurring when looking at lines on chart paper within the macular area, or central 1.0 degree of visual arc. Usually it occurs in one eye first, and may cause binocular diplopia or double vision if the image from one eye is too different from the image of the other eye. The distortions can make objects look different in size, especially in the central portion of the visual field, creating a localized or field dependent aniseikonia that cannot be fully corrected optically with glasses. Partial correction often improves the binocular vision considerably though. In the young, these cells occasionally pull free and disintegrate on their own; but in the majority of those affected the condition is permanent. The underlying photoreceptor cells, rod cells and cone cells, are usually not damaged unless the membrane becomes quite thick and hard; so usually there is no macular degeneration.

Idiopathic orbital inflammatory (IOI) disease refers to a marginated mass-like enhancing soft tissue involving any area of the orbit. It is the most common painful orbital mass in the adult population, and is associated with proptosis, cranial nerve palsy, uveitis, and retinal detachment. Idiopathic orbital inflammatory syndrome, also known as orbital pseudotumor, was first described by Gleason in 1903 and by Busse and Hochheim. It was then characterized as a distinct entity in 1905 by Birch-Hirschfeld. It is a benign, nongranulomatous orbital inflammatory process characterized by extraocular orbital and adnexal inflammation with no known local or systemic cause. Its diagnosis is of exclusion once neoplasm, primary infection and systemic disorders have been ruled out. Once diagnosed, it is characterized by its chronicity, anatomic location or histologic subtype.

Retinal vasculitis is inflammation of the vascular branches of the retinal artery, caused either by primary ocular disease processes, or as a specific presentation of any systemic form of vasculitis such as Behçet's disease, sarcoidosis, multiple sclerosis, or any form of systemic necrotizing vasculitis such as temporal arteritis, polyarteritis nodosa, and granulomatosis with polyangiitis, or due to lupus erythematosus, or rheumatoid arthritis. Eales disease, pars planitis, birdshot retinochoroidopathy, and Fuchs heterochromic iridocyclitis (FHI) can also cause retinal vasculitis. Infectious pathogens such as Mycobacterium tuberculosis, visceral larva migrans can also cause retinal vasculitis.

Branch retinal vein occlusion is a common retinal vascular disease of the elderly. It is caused by the occlusion of one of the branches of central retinal vein.

Vitreomacular adhesion (VMA) is a human medical condition where the vitreous gel of the human eye adheres to the retina in an abnormally strong manner. As the eye ages, it is common for the vitreous to separate from the retina. But if this separation is not complete, i.e. there is still an adhesion, this can create pulling forces on the retina that may result in subsequent loss or distortion of vision. The adhesion in of itself is not dangerous, but the resulting pathological vitreomacular traction (VMT) can cause severe ocular damage.
Vogt–Koyanagi–Harada disease (VKH) is a multisystem disease of presumed autoimmune cause that affects melanin-pigmented tissues. The most significant manifestation is bilateral, diffuse uveitis, which affects the eyes. VKH may variably also involve the inner ear, with effects on hearing, the skin, and the meninges of the central nervous system.
Intravitreal injection is the method of administration of drugs into the eye by injection with a fine needle. The medication will be directly applied into the vitreous humor. It is used to treat various eye diseases, such as age-related macular degeneration (AMD), diabetic retinopathy, and infections inside the eye such as endophthalmitis. As compared to topical administration, this method is beneficial for a more localized delivery of medications to the targeted site, as the needle can directly pass through the anatomical eye barrier and dynamic barrier. It could also minimize adverse drug effect to other body tissues via the systemic circulation, which could be a possible risk for intravenous injection of medications. Although there are risks of infections or other complications, with suitable precautions throughout the injection process, chances for these complications could be lowered.
Sickle cell retinopathy can be defined as retinal changes due to blood vessel damage in the eye of a person with a background of sickle cell disease. It can likely progress to loss of vision in late stages due to vitreous hemorrhage or retinal detachment. Sickle cell disease is a structural red blood cell disorder leading to consequences in multiple systems. It is characterized by chronic red blood cell destruction, vascular injury, and tissue ischemia causing damage to the brain, eyes, heart, lungs, kidneys, spleen, and musculoskeletal system.

Secondary glaucoma is a collection of progressive optic nerve disorders associated with a rise in intraocular pressure (IOP) which results in the loss of vision. In clinical settings, it is defined as the occurrence of IOP above 21 mmHg requiring the prescription of IOP-managing drugs. It can be broadly divided into two subtypes: secondary open-angle glaucoma and secondary angle-closure glaucoma, depending on the closure of the angle between the cornea and the iris. Principal causes of secondary glaucoma include optic nerve trauma or damage, eye disease, surgery, neovascularization, tumours and use of steroid and sulfa drugs. Risk factors for secondary glaucoma include uveitis, cataract surgery and also intraocular tumours. Common treatments are designed according to the type and the underlying causative condition, in addition to the consequent rise in IOP. These include drug therapy, the use of miotics, surgery or laser therapy.
Schwartz–Matsuo syndrome is a human eye disease characterised by rhegmatogenous retinal detachment, elevated intraocular pressure (IOP) and open angle of anterior chamber.

Uveitic glaucoma is most commonly a progression stage of noninfectious anterior uveitis or iritis.