Eye surgery, also known as ophthalmic surgery or ocular surgery, is surgery performed on the eye or its adnexa. Eye surgery is part of ophthalmology and is performed by an ophthalmologist or eye surgeon. The eye is a fragile organ, and requires due care before, during, and after a surgical procedure to minimize or prevent further damage. An eye surgeon is responsible for selecting the appropriate surgical procedure for the patient, and for taking the necessary safety precautions. Mentions of eye surgery can be found in several ancient texts dating back as early as 1800 BC, with cataract treatment starting in the fifth century BC. It continues to be a widely practiced class of surgery, with various techniques having been developed for treating eye problems.

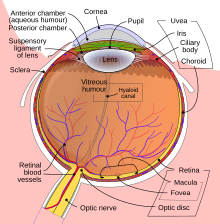
The aqueous humour is a transparent water-like fluid similar to blood plasma, but containing low protein concentrations. It is secreted from the ciliary body, a structure supporting the lens of the eyeball. It fills both the anterior and the posterior chambers of the eye, and is not to be confused with the vitreous humour, which is located in the space between the lens and the retina, also known as the posterior cavity or vitreous chamber. Blood cannot normally enter the eyeball.

Phacoemulsification is a cataract surgery method in which the internal lens of the eye which has developed a cataract is emulsified with the tip of an ultrasonic handpiece and aspirated from the eye. Aspirated fluids are replaced with irrigation of balanced salt solution to maintain the volume of the anterior chamber during the procedure. This procedure minimises the incision size and reduces the recovery time and risk of surgery induced astigmatism.

An Intraocular lens (IOL) is a lens implanted in the eye usually as part of a treatment for cataracts or for correcting other vision problems such as short sightedness and long sightedness, a form of refractive surgery. If the natural lens is left in the eye, the IOL is known as phakic, otherwise it is a pseudophakic lens. Both kinds of IOLs are designed to provide the same light-focusing function as the natural crystalline lens. This can be an alternative to LASIK, but LASIK is not an alternative to an IOL for treatment of cataracts.

A phakic intraocular lens (PIOL) is a special kind of intraocular lens that is implanted surgically into the eye to correct myopia (nearsightedness). It is called "phakic" because the eye's natural lens is left untouched. Intraocular lenses that are implanted into eyes after the eye's natural lens has been removed during cataract surgery are known as pseudophakic.

The corneal endothelium is a single layer of endothelial cells on the inner surface of the cornea. It faces the chamber formed between the cornea and the iris.

Physical or chemical injuries of the eye can be a serious threat to vision if not treated appropriately and in a timely fashion. The most obvious presentation of ocular (eye) injuries is redness and pain of the affected eyes. This is not, however, universally true, as tiny metallic projectiles may cause neither symptom. Tiny metallic projectiles should be suspected when a patient reports metal on metal contact, such as with hammering a metal surface. Corneal foreign body is one of the most common preventable occupational hazard. Intraocular foreign bodies do not cause pain because of the lack of nerve endings in the vitreous humour and retina that can transmit pain sensations. As such, general or emergency department doctors should refer cases involving the posterior segment of the eye or intraocular foreign bodies to an ophthalmologist. Ideally, ointment would not be used when referring to an ophthalmologist, since it diminishes the ability to carry out a thorough eye examination.

A red eye is an eye that appears red due to illness or injury. It is usually injection and prominence of the superficial blood vessels of the conjunctiva, which may be caused by disorders of these or adjacent structures. Conjunctivitis and subconjunctival hemorrhage are two of the less serious but more common causes.

The anterior chamber (AC) is the aqueous humor-filled space inside the eye between the iris and the cornea's innermost surface, the endothelium. Hyphema, anterior uveitis and glaucoma are three main pathologies in this area. In hyphema, blood fills the anterior chamber as a result of a hemorrhage, most commonly after a blunt eye injury. Anterior uveitis is an inflammatory process affecting the iris and ciliary body, with resulting inflammatory signs in the anterior chamber. In glaucoma, blockage of the trabecular meshwork prevents the normal outflow of aqueous humour, resulting in increased intraocular pressure, progressive damage to the optic nerve head, and eventually blindness.

A corneal ulcer, or ulcerative keratitis, is an inflammatory condition of the cornea involving loss of its outer layer. It is very common in dogs and is sometimes seen in cats. In veterinary medicine, the term corneal ulcer is a generic name for any condition involving the loss of the outer layer of the cornea, and as such is used to describe conditions with both inflammatory and traumatic causes.
Iridocorneal endothelial (ICE) syndromes are a spectrum of diseases characterized by slowly progressive abnormalities of the corneal endothelium and features including corneal edema, iris distortion, and secondary angle-closure glaucoma. ICE syndromes are predominantly unilateral and nonhereditary. The condition occurs in predominantly middle-aged women.

Iridodialysis is a localized separation or tearing away of the iris from its attachment to the ciliary body.

Buphthalmos is enlargement of the eyeball and is most commonly seen in infants and young children. It is sometimes referred to as buphthalmia. It usually appears in the newborn period or the first 3 months of life. and in most cases indicates the presence of congenital (infantile) glaucoma, which is a disorder in which elevated pressures within the eye lead to structural eye damage and vision loss.

Intraocular hemorrhage is bleeding inside the eye. Bleeding can occur from any structure of the eye where there is vasculature or blood flow, including the anterior chamber, vitreous cavity, retina, choroid, suprachoroidal space, or optic disc.
Fuchs heterochromic iridocyclitis (FHI) is a chronic unilateral uveitis appearing with the triad of heterochromia, predisposition to cataract and glaucoma, and keratitic precipitates on the posterior corneal surface. Patients are often asymptomatic and the disease is often discovered through investigation of the cause of the heterochromia or cataract. Neovascularisation is possible and any eye surgery, such as cataract surgery, can cause bleeding from the fragile vessels in the atrophic iris causing accumulation of blood in the anterior chamber of the eye, also known as hyphema.
The Trabectome is a surgical device that can be used for ab interno trabeculotomy, a minimally invasive glaucoma surgery for the surgical management of adult, juvenile, and infantile glaucoma. The trabecular meshwork is a major site of resistance to aqueous humor outflow. As angle surgeries such as Trabectome follow the physiologic outflow pathway, the risk of complications is significantly lower than filtering surgeries. Hypotony with damage to the macula, can occur with pressures below 5 mmHg, for instance, after traditional trabeculectomy, because of the episcleral venous pressure limit. The Trabectome handpiece is inserted into the anterior chamber, its tip positioned into Schlemm's canal, and advanced to the left and to the right. Different from cautery, the tip generates plasma to molecularize the trabecular meshwork and remove it drag-free and with minimal thermal effect. Active irrigation of the trabectome surgery system helps to keep the anterior chamber formed during the procedure and precludes the need for ophthalmic viscoelastic devices. Viscoelastic devices tend to trap debris or gas bubbles and diminish visualization. The Trabectome decreases the intra-ocular pressure typically to a mid-teen range and reduces the patient's requirement to take glaucoma eye drops and glaucoma medications. The theoretically lowest pressure that can be achieved is equal to 8 mmHg in the episcleral veins. This procedure is performed through a small incision and can be done on an outpatient basis.

Corneal opacification is a term used when the human cornea loses its transparency. The term corneal opacity is used particularly for the loss of transparency of cornea due to scarring. Transparency of the cornea is dependent on the uniform diameter and the regular spacing and arrangement of the collagen fibrils within the stroma. Alterations in the spacing of collagen fibrils in a variety of conditions including corneal edema, scars, and macular corneal dystrophy is clinically manifested as corneal opacity. The term corneal blindness is commonly used to describe blindness due to corneal opacity.
Uveitis–glaucoma–hyphaema (UGH) syndrome, also known as Ellingson syndrome, is a complication of cataract surgery, caused by intraocular lens subluxation or dislocation. The chafing of mispositioned intraocular lens over iris, ciliary body or iridocorneal angle cause elevated intraocular pressure (IOP) anterior uveitis and hyphema. It is most commonly caused by anterior chamber IOLs and sulcus IOLs but, the condition can be seen with any type of IOL, including posterior chamber lenses and cosmetic iris implants.
Ghost cell glaucoma (GCG) is a type of secondary glaucoma occurs due to long standing vitreous hemorrhage. The rigid and less pliable degenerated red blood cells block the trabecular meshwork and increase the pressure inside eyes.
Anterior chamber paracentesis (ACP) is a surgical procedure done to reduce intraocular pressure (IOP) of the eye. The procedure is used in management of glaucoma and uveitis. It is also used for clinical diagnosis of infectious uveitis.