In biology, hemostasis or haemostasis is a process to prevent and stop bleeding, meaning to keep blood within a damaged blood vessel. It is the first stage of wound healing. This involves coagulation, which changes blood from a liquid to a gel. Intact blood vessels are central to moderating blood's tendency to form clots. The endothelial cells of intact vessels prevent blood clotting with a heparin-like molecule and thrombomodulin, and prevent platelet aggregation with nitric oxide and prostacyclin. When endothelium of a blood vessel is damaged, the endothelial cells stop secretion of coagulation and aggregation inhibitors and instead secrete von Willebrand factor, which initiate the maintenance of hemostasis after injury. Hemostasis involves three major steps:

Haemophilia C (also known as plasma thromboplastin antecedent deficiency or Rosenthal syndrome) is a mild form of haemophilia affecting both sexes, due to factor XI deficiency. It predominantly occurs in Ashkenazi Jews. It is the fourth most common coagulation disorder after von Willebrand's disease and haemophilia A and B. In the United States, it is thought to affect 1 in 100,000 of the adult population, making it 10% as common as haemophilia A.

Dense granules are specialized secretory organelles. Dense granules are found only in platelets and are smaller than alpha granules. The origin of these dense granules is still unknown, however, it is thought that may come from the mechanism involving the endocytotic pathway. Dense granules are a sub group of lysosome-related organelles (LRO). There are about three to eight of these in a normal human platelet.

Chédiak–Higashi syndrome (CHS) is a rare autosomal recessive disorder that arises from a mutation of a lysosomal trafficking regulator protein, which leads to a decrease in phagocytosis. The decrease in phagocytosis results in recurrent pyogenic infections, albinism, and peripheral neuropathy.
Severe congenital neutropenia (SCN), also often known as Kostmann syndrome or disease, is a group of rare disorders that affect myelopoiesis, causing a congenital form of neutropenia, usually without other physical malformations. SCN manifests in infancy with life-threatening bacterial infections.

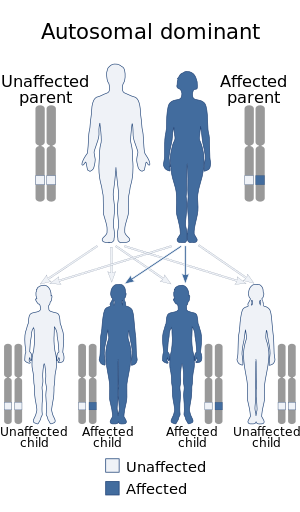
Hypoprothrombinemia is a rare blood disorder in which a deficiency in immunoreactive prothrombin, produced in the liver, results in an impaired blood clotting reaction, leading to an increased physiological risk for spontaneous bleeding. This condition can be observed in the gastrointestinal system, cranial vault, and superficial integumentary system, affecting both the male and female population. Prothrombin is a critical protein that is involved in the process of hemostasis, as well as illustrating procoagulant activities. This condition is characterized as an autosomal recessive inheritance congenital coagulation disorder affecting 1 per 2,000,000 of the population, worldwide, but is also attributed as acquired.

Heřmanský–Pudlák syndrome is an extremely rare autosomal recessive disorder which results in oculocutaneous albinism, bleeding problems due to a platelet abnormality, and storage of an abnormal fat-protein compound. It is considered to affect around 1 in 500,000 people worldwide, with a significantly higher occurrence in Puerto Ricans, with a prevalence of 1 in 1800. Many of the clinical research studies on the disease have been conducted in Puerto Rico.

Bernard–Soulier syndrome (BSS) is a rare autosomal recessive bleeding disorder that is caused by a deficiency of the glycoprotein Ib-IX-V complex (GPIb-IX-V), the receptor for von Willebrand factor. The incidence of BSS is estimated to be less than 1 case per million persons, based on cases reported from Europe, North America, and Japan. BSS is a giant platelet disorder, meaning that it is characterized by abnormally large platelets.

Ristocetin is a glycopeptide antibiotic, obtained from Amycolatopsis lurida, previously used to treat staphylococcal infections. It is no longer used clinically because it caused thrombocytopenia and platelet agglutination. It is now used solely to assay those functions in vitro in the diagnosis of conditions such as von Willebrand disease (vWD) and Bernard–Soulier syndrome. Platelet agglutination caused by ristocetin can occur only in the presence of von Willebrand factor multimers, so if ristocetin is added to blood lacking the factor, the platelets will not clump.

Griscelli syndrome is a rare autosomal recessive disorder characterized by albinism (hypopigmentation) with immunodeficiency, that usually causes death by early childhood. Researchers have developed three different classifications of the form of disorder, characterised by different signs and symptoms. Type 1 Griscelli Syndrome is assosciated with severe brain function issues along with distinctive discolouring of the hair and skin. Type 2 Griscelli Syndrome have immune system abnormalities in addition to hypopigmentation of skin and hair. Finally, Type 3 is seen as those only affected by hypopigmentation of the skin and hair. This type is not associated with immune deficiencies or neurological abnormalities.

Gray platelet syndrome (GPS), or platelet alpha-granule deficiency, is a rare congenital autosomal recessive bleeding disorder caused by a reduction or absence of alpha-granules in blood platelets, and the release of proteins normally contained in these granules into the marrow, causing myelofibrosis. The name derives from the initial observation of gray appearance of platelets with a paucity of granules on blood films from a patient with a lifelong bleeding disorder.

Hermansky–Pudlak syndrome 1 protein is a protein that in humans is encoded by the HPS1 gene.

Hermansky–Pudlak syndrome 4 protein is a protein that in humans is encoded by the HPS4 gene.

Hermansky–Pudlak syndrome 3 protein is a protein that in humans is encoded by the HPS3 gene.

Hermansky–Pudlak syndrome 5 protein is a protein that in humans is encoded by the HPS5 gene.

Hermansky–Pudlak syndrome 6 (HPS6), also known as ruby-eye protein homolog (Ru), is a protein that in humans is encoded by the HPS6 gene.
Cerebral dysgenesis–neuropathy–ichthyosis–keratoderma syndrome is a neurocutaneous condition caused by mutation in the SNAP29 gene.

Giant platelet disorders, also known as macrothrombocytopenia, are rare disorders featuring abnormally large platelets, thrombocytopenia and a tendency to bleeding. Giant platelets cannot stick adequately to an injured blood vessel walls, resulting in abnormal bleeding when injured. Giant platelet disorder occurs for inherited diseases like Bernard–Soulier syndrome, gray platelet syndrome and May–Hegglin anomaly.

Lyngstadaas syndrome, also known as severe dental aberrations in familial steroid dehydrogenase deficiency, is a rare autosomal recessive liver disease involving an enzyme deficiency and dental anomalies. The disease is named after the Norwegian professor Ståle Petter Lyngstadaas.