Haemophilia, or hemophilia, is a mostly inherited genetic disorder that impairs the body's ability to make blood clots, a process needed to stop bleeding. This results in people bleeding for a longer time after an injury, easy bruising, and an increased risk of bleeding inside joints or the brain. Those with a mild case of the disease may have symptoms only after an accident or during surgery. Bleeding into a joint can result in permanent damage while bleeding in the brain can result in long term headaches, seizures, or a decreased level of consciousness.

Haemophilia A is a blood clotting disorder caused by a genetic deficiency in clotting factor VIII, thereby resulting in significant susceptibility to bleeding, both internally and externally. This condition occurs almost exclusively in males born to carrier mothers due to X-linked recessive inheritance. Nevertheless, rare isolated cases do emerge from de novo (spontaneous) mutations.

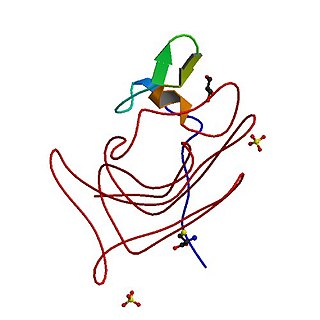
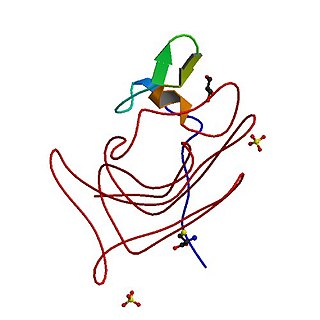
Von Willebrand disease (VWD) is the most common hereditary blood-clotting disorder in humans. An acquired form can sometimes result from other medical conditions. It arises from a deficiency in the quality or quantity of von Willebrand factor (VWF), a multimeric protein that is required for platelet adhesion. It is known to affect several breeds of dogs as well as humans. The three forms of VWD are hereditary, acquired, and pseudo or platelet type. The three types of hereditary VWD are VWD type 1, VWD type 2, and VWD type 3. Type 2 contains various subtypes. Platelet type VWD is also an inherited condition.

Haemophilia C (also known as plasma thromboplastin antecedent deficiency or Rosenthal syndrome) is a mild form of haemophilia affecting both sexes, due to factor XI deficiency. It predominantly occurs in Ashkenazi Jews. It is the fourth most common coagulation disorder after von Willebrand's disease and haemophilia A and B. In the United States, it is thought to affect 1 in 100,000 of the adult population, making it 10% as common as haemophilia A.

In medicine (hematology), bleeding diathesis is an unusual susceptibility to bleed (hemorrhage) mostly due to hypocoagulability, in turn caused by a coagulopathy. Therefore, this may result in the reduction of platelets being produced and leads to excessive bleeding. Several types of coagulopathy are distinguished, ranging from mild to lethal. Coagulopathy can be caused by thinning of the skin, such that the skin is weakened and is bruised easily and frequently without any trauma or injury to the body. Also, coagulopathy can be contributed by impaired wound healing or impaired clot formation.

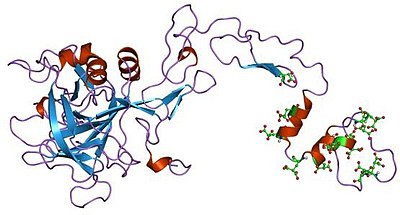
Coagulation factor VII is one of the proteins that causes blood to clot in the coagulation cascade, and in humans is coded for by the gene F7. It is an enzyme of the serine protease class. Once bound to tissue factor released from damaged tissues, it is converted to factor VIIa, which in turn activates factor IX and factor X.

Factor IX is one of the serine proteases of the coagulation system; it belongs to peptidase family S1. Deficiency of this protein causes haemophilia B. It was discovered in 1952 after a young boy named Stephen Christmas was found to be lacking this exact factor, leading to haemophilia.

Fresh frozen plasma (FFP) is a blood product made from the liquid portion of whole blood. It is used to treat conditions in which there are low blood clotting factors or low levels of other blood proteins. It may also be used as the replacement fluid in plasma exchange. Using ABO compatible plasma, while not required, may be recommended. Use as a volume expander is not recommended. It is given by slow injection into a vein.
Congenital afibrinogenemia is a rare, genetically inherited blood fibrinogen disorder in which the blood does not clot normally due to the lack of fibrinogen, a blood protein necessary for coagulation. This disorder is autosomal recessive, meaning that two unaffected parents can have a child with the disorder. The lack of fibrinogen expresses itself with excessive and, at times, uncontrollable bleeding.

Hypoprothrombinemia is a rare blood disorder in which a deficiency in immunoreactive prothrombin, produced in the liver, results in an impaired blood clotting reaction, leading to an increased physiological risk for spontaneous bleeding. This condition can be observed in the gastrointestinal system, cranial vault, and superficial integumentary system, affecting both the male and female population. Prothrombin is a critical protein that is involved in the process of hemostasis, as well as illustrating procoagulant activities. This condition is characterized as an autosomal recessive inheritance congenital coagulation disorder affecting 1 per 2,000,000 of the population, worldwide, but is also attributed as acquired.

Factor X deficiency is a bleeding disorder characterized by a lack in the production of factor X (FX), an enzyme protein that causes blood to clot in the coagulation cascade. Produced in the liver FX when activated cleaves prothrombin to generate thrombin in the intrinsic pathway of coagulation. This process is vitamin K dependent and enhanced by activated factor V.

Factor VII deficiency is a bleeding disorder characterized by a lack in the production of Factor VII (FVII) (proconvertin), a protein that causes blood to clot in the coagulation cascade. After a trauma factor VII initiates the process of coagulation in conjunction with tissue factor in the extrinsic pathway.

Factor VIII is a medication used to treat and prevent bleeding in people with hemophilia A and other causes of low factor VIII. Certain preparations may also be used in those with von Willebrand's disease. It is given by slow injection into a vein.
Octapharma AG, founded in 1983, is a family-owned pharmaceutical company based in Switzerland. It bills itself as "one of the largest human protein manufacturers in the world, developing and producing human proteins from human plasma and human cell lines."
Moroctocog alfa is a recombinant antihemophilic factor genetically engineered from Chinese hamster ovary (CHO) cell line. Chemically it is a glycoprotein. It is manufactured by Genetics Institute, Inc. and used to control and prevent hemorrhagic bleeding and prophylaxis associated with surgery or to reduce the number of spontaneous bleeding episodes in patients with hemophilia A. It is partially a recombinant coagulation factor VIII since it has an amino acid sequence which compares to the 90 + 80 kDa form of factor VIII (BDDrFVIII). It also has posttranslational modifications which are similar to those of the plasma-derived molecule. It can not prevent hemorrhagic bleeding associated with von Willebrand's disease since it is not a von Willebrand factor.
Recombinant factor VIIa, also known as eptacog alfa (INN), and sold under the brand name Novoseven, among others, is a form of blood factor VII that has been manufactured via recombinant technology. It is administered via an injection into a vein.

Jeanne Marie Lusher, M.D. was an American physician, pediatric hematologist/oncologist, and a researcher in the field of bleeding disorders of childhood, and has served as the director of Hemostasis Program at the Children's Hospital of Michigan until her retirement on June 28, 2013.
Factor XII deficiency is a deficiency in the production of factor XII (FXII), a plasma glycoprotein and clotting factor that participates in the coagulation cascade and activates factor XI. FXII appears to be not essential for blood clotting, as individuals with this condition are usually asymptomatic and form blood clots in vivo. FXII deficiency tends to be identified during presurgical laboratory screening for bleeding disorders.
Acquired haemophilia A (AHA) is a rare but potentially life-threatening bleeding disorder characterized by autoantibodies directed against coagulation factor VIII. These autoantibodies constitute the most common spontaneous inhibitor to any coagulation factor and may induce spontaneous bleeding in patients with no previous history of a bleeding disorder.
Etranacogene dezaparvovec, sold under the brand name Hemgenix is a gene therapy used for the treatment of hemophilia B. Etranacogene dezaparvovec is an adeno-associated virus vector-based gene therapy which consists of a viral vector carrying a gene for clotting Factor IX. The gene is expressed in the liver to produce Factor IX protein, to increase blood levels of Factor IX and thereby limit bleeding episodes. Hemophilia B is a genetic bleeding disorder resulting from missing or insufficient levels of blood clotting Factor IX, a protein needed to produce blood clots to stop bleeding.