Related Research Articles

Conjunctivitis, also known as pink eye, is inflammation of the outermost layer of the white part of the eye and the inner surface of the eyelid. It makes the eye appear pink or reddish. Pain, burning, scratchiness, or itchiness may occur. The affected eye may have increased tears or be "stuck shut" in the morning. Swelling of the white part of the eye may also occur. Itching is more common in cases due to allergies. Conjunctivitis can affect one or both eyes.

The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber. Along with the anterior chamber and lens, the cornea refracts light, accounting for approximately two-thirds of the eye's total optical power. In humans, the refractive power of the cornea is approximately 43 dioptres. The cornea can be reshaped by surgical procedures such as LASIK.

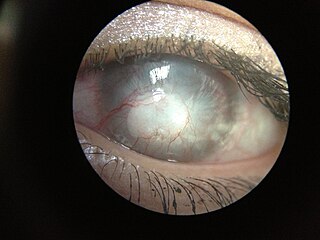
A pterygium of the eye is a pinkish, roughly triangular tissue growth of the conjunctiva onto the cornea of the eye. It typically starts on the cornea near the nose. It may slowly grow but rarely grows so large that it covers the pupil and impairs vision. Often both eyes are involved.

Eye surgery, also known as ophthalmic or ocular surgery, is surgery performed on the eye or its adnexa, by an ophthalmologist. Eye surgery is part of ophthalmology. The eye is a fragile organ, and requires due care before, during, and after a surgical procedure to minimize or prevent further damage. An eye surgeon is responsible for selecting the appropriate surgical procedure for the patient, and for taking the necessary safety precautions. Mentions of eye surgery can be found in several ancient texts dating back as early as 1800 BC, with cataract treatment starting in the fifth century BC. It continues to be a widely practiced class of surgery, with various techniques having been developed for treating eye problems.
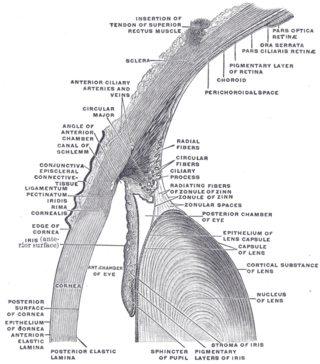
The conjunctiva is a thin mucous membrane that lines the inside of the eyelids and covers the sclera. It is composed of non-keratinized, stratified squamous epithelium with goblet cells, stratified columnar epithelium and stratified cuboidal epithelium. The conjunctiva is highly vascularised, with many microvessels easily accessible for imaging studies.

A red eye is an eye that appears red due to illness or injury. It is usually injection and prominence of the superficial blood vessels of the conjunctiva, which may be caused by disorders of these or adjacent structures. Conjunctivitis and subconjunctival hemorrhage are two of the less serious but more common causes.

Xerophthalmia is a medical condition in which the eye fails to produce tears. It may be caused by vitamin A deficiency, which is sometimes used to describe that condition, although there may be other causes.
Ocular melanosis (OM) is a blue-gray and/or brown lesion of the conjunctiva that can be separated into benign conjunctival epithelial melanosis (BCEM) and primary acquired melanosis (PAM), of which the latter is considered a risk factor for uveal melanoma. The disease is caused by an increase of melanocytes in the iris, choroid, and surrounding structures. Overproduction of pigment by these cells can block the trabecular meshwork through which fluid drains from the eye. The increased fluid in the eye leads to increased pressure, which can lead to glaucoma. In humans, this is sometimes known as pigment dispersion syndrome.

Vernal keratoconjunctivitis is a recurrent, bilateral, and self-limiting type of conjunctivitis having a periodic seasonal incidence.

A pinguecula is a common type of conjunctival stromal degeneration in the eye. It appears as an elevated yellow-white plaque in the bulbar conjunctiva near the limbus. Calcification may also seen occasionally.
Corneal neovascularization (CNV) is the in-growth of new blood vessels from the pericorneal plexus into avascular corneal tissue as a result of oxygen deprivation. Maintaining avascularity of the corneal stroma is an important aspect of corneal pathophysiology as it is required for corneal transparency and optimal vision. A decrease in corneal transparency causes visual acuity deterioration. Corneal tissue is avascular in nature and the presence of vascularization, which can be deep or superficial, is always pathologically related.

Corneal ulcer, also called keratitis, is an inflammatory or, more seriously, infective condition of the cornea involving disruption of its epithelial layer with involvement of the corneal stroma. It is a common condition in humans particularly in the tropics and in farming. In developing countries, children afflicted by vitamin A deficiency are at high risk for corneal ulcer and may become blind in both eyes persisting throughout life. In ophthalmology, a corneal ulcer usually refers to having an infection, while the term corneal abrasion refers more to a scratch injury.

The corneal limbus is the border between the cornea and the sclera. It contains limbal stem cells in its palisades of Vogt. It may be affected by cancer or aniridia, among other issues. The limbal ring is a visible dark ring around the iris of the eye composed of darkened areas of the corneal limbus.

Pterygium refers to any wing-like triangular membrane occurring in the neck, eyes, knees, elbows, ankles or digits.

Conjunctivochalasis, also known as Mechanical Dry Eye (MDE), is a common eye surface condition characterized by the presence of excess folds of the conjunctiva located between the globe of the eye and the eyelid margin.
Conjunctival squamous cell carcinoma and corneal intraepithelial neoplasia comprise ocular surface squamous neoplasia (OSSN). SCC is the most common malignancy of the conjunctiva in the US, with a yearly incidence of 1–2.8 per 100,000. Risk factors for the disease are exposure to sun, exposure to UVB, and light-colored skin. Other risk factors include radiation, smoking, HPV, arsenic, and exposure to polycyclic hydrocarbons.
Mooren's ulcer is a rare idiopathic ocular disorder that may lead to blindness due to progressive destruction of the peripheral cornea. Although the etiology of Mooren's ulcer is poorly understood, recent evidence suggests that the pathogenesis of this disease appears to be the result of an autoimmune process directed against molecules expressed in the corneal stroma.

The human cornea is a transparent membrane which allows light to pass through it. The word corneal opacification literally means loss of normal transparency of cornea. The term corneal opacity is used particularly for the loss of transparency of cornea due to scarring. Transparency of the cornea is dependent on the uniform diameter and the regular spacing and arrangement of the collagen fibrils within the stroma. Alterations in the spacing of collagen fibrils in a variety of conditions including corneal edema, scars, and macular corneal dystrophy is clinically manifested as corneal opacity. The term corneal blindness is commonly used to describe blindness due to corneal opacity.
Ankyloblepharon is defined as the adhesion of the edges of the upper eyelid with the lower eyelid. Ankyloblepharon must be differentiated from blepharophimosis, in which palpebral aperture is reduced and there is telecanthus, but the eyelid margins are normal. Another condition similar to ankyloblepharon is symblepharon, in which the palpebral conjunctiva is attached to the bulbar conjunctiva. Recognition of ankyloblepharon necessitates systemic examination to detect associated abnormalities such as genitourinary and cardiac abnormalities and syndactyly.
Exposure keratopathy is medical condition affecting the cornea of eyes. It can lead to corneal ulceration and permanent loss of vision due to corneal opacity.
References
- ↑ Prabhakar, Srinivasapuram Krishnachary (October 2014). "Safety profile and complications of autologous limbal conjunctival transplantation for primary pterygium". Saudi Journal of Ophthalmology. 28 (4): 262–267. doi: 10.1016/j.sjopt.2014.03.006 . ISSN 1319-4534. PMC 4250486 . PMID 25473341.
- ↑ "Pseudopterygium | Columbia Ophthalmology". www.columbiaeye.org.
- 1 2 3 John F, Salmon (13 December 2019). "Conjunctiva". Kanski's clinical ophthalmology : a systematic approach (9th ed.). Elsevier. pp. 198–199. ISBN 978-0-7020-7711-1.
- 1 2 "Volume 6, Chapter 35. Pterygium". www.oculist.net.
- 1 2 3 Khurana, AK (31 August 2015). "Diseases of conjunctiva". Comprehensive ophthalmology (6th ed.). Jaypee Brothers. p. 88. ISBN 978-93-5152-657-5.
- ↑ HV, Nema; Nithin, Nema (December 2008). Textbook of ophthalmology (5th ed.). Jaypee Brothers. ISBN 978-81-8448-307-9.