Positron emission tomography (PET) is a functional imaging technique that uses radioactive substances known as radiotracers to visualize and measure changes in metabolic processes, and in other physiological activities including blood flow, regional chemical composition, and absorption. Different tracers are used for various imaging purposes, depending on the target process within the body.

Radiology is the medical specialty that uses medical imaging to diagnose diseases and guide their treatment, within the bodies of humans and other animals. It began with radiography, but today it includes all imaging modalities, including those that use no ionizing electromagnetic radiation, as well as others that do, such as computed tomography (CT), fluoroscopy, and nuclear medicine including positron emission tomography (PET). Interventional radiology is the performance of usually minimally invasive medical procedures with the guidance of imaging technologies such as those mentioned above.
Medical physics deals with the application of the concepts and methods of physics to the prevention, diagnosis and treatment of human diseases with a specific goal of improving human health and well-being. Since 2008, medical physics has been included as a health profession according to International Standard Classification of Occupation of the International Labour Organization.

Single-photon emission computed tomography is a nuclear medicine tomographic imaging technique using gamma rays. It is very similar to conventional nuclear medicine planar imaging using a gamma camera, but is able to provide true 3D information. This information is typically presented as cross-sectional slices through the patient, but can be freely reformatted or manipulated as required.

Nuclear medicine or nucleology is a medical specialty involving the application of radioactive substances in the diagnosis and treatment of disease. Nuclear imaging, in a sense, is "radiology done inside out" because it records radiation emitted from within the body rather than radiation that is transmitted through the body from external sources like X-ray generators. In addition, nuclear medicine scans differ from radiology, as the emphasis is not on imaging anatomy, but on the function. For such reason, it is called a physiological imaging modality. Single photon emission computed tomography (SPECT) and positron emission tomography (PET) scans are the two most common imaging modalities in nuclear medicine.
A radioligand is a microscopic particle which consists of a therapeutic radioactive isotope and the cell-targeting compound - the ligand. The ligand is the target binding site, it may be on the surface of the targeted cancer cell for therapeutic purposes. Radioisotopes can occur naturally or be synthesized and produced in a cyclotron/nuclear reactor. The different types of radioisotopes include Y-90, H-3, C-11, Lu-177, Ac-225, Ra-223, In-111, I-131, I-125, etc. Thus, radioligands must be produced in special nuclear reactors for the radioisotope to remain stable. Radioligands can be used to analyze/characterize receptors, to perform binding assays, to help in diagnostic imaging, and to provide targeted cancer therapy. Radiation is a novel method of treating cancer and is effective in short distances along with being unique/personalizable and causing minimal harm to normal surrounding cells. Furthermore, radioligand binding can provide information about receptor-ligand interactions in vitro and in vivo. Choosing the right radioligand for the desired application is important. The radioligand must be radiochemically pure, stable, and demonstrate a high degree of selectivity, and high affinity for their target.

Scintigraphy, also known as a gamma scan, is a diagnostic test in nuclear medicine, where radioisotopes attached to drugs that travel to a specific organ or tissue (radiopharmaceuticals) are taken internally and the emitted gamma radiation is captured by gamma cameras, which are external detectors that form two-dimensional images in a process similar to the capture of x-ray images. In contrast, SPECT and positron emission tomography (PET) form 3-dimensional images and are therefore classified as separate techniques from scintigraphy, although they also use gamma cameras to detect internal radiation. Scintigraphy is unlike a diagnostic X-ray where external radiation is passed through the body to form an image.

Iodine-131 is an important radioisotope of iodine discovered by Glenn Seaborg and John Livingood in 1938 at the University of California, Berkeley. It has a radioactive decay half-life of about eight days. It is associated with nuclear energy, medical diagnostic and treatment procedures, and natural gas production. It also plays a major role as a radioactive isotope present in nuclear fission products, and was a significant contributor to the health hazards from open-air atomic bomb testing in the 1950s, and from the Chernobyl disaster, as well as being a large fraction of the contamination hazard in the first weeks in the Fukushima nuclear crisis. This is because 131I is a major fission product of uranium and plutonium, comprising nearly 3% of the total products of fission. See fission product yield for a comparison with other radioactive fission products. 131I is also a major fission product of uranium-233, produced from thorium.

There are 37 known isotopes of iodine (53I) from 108I to 144I; all undergo radioactive decay except 127I, which is stable. Iodine is thus a monoisotopic element.
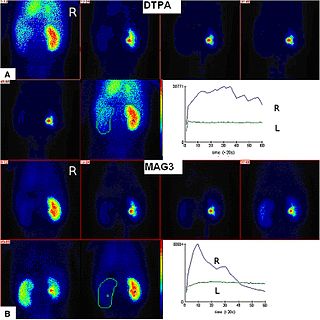
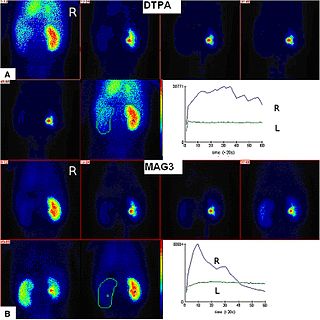
Radioisotope renography is a form of medical imaging of the kidneys that uses radiolabelling. A renogram, which may also be known as a MAG3 scan, allows a nuclear medicine physician or a radiologist to visualize the kidneys and learn more about how they are functioning. MAG3 is an acronym for mercapto acetyl tri glycine, a compound that is chelated with a radioactive element – technetium-99m.
Iodine-123 (123I) is a radioactive isotope of iodine used in nuclear medicine imaging, including single-photon emission computed tomography (SPECT) or SPECT/CT exams. The isotope's half-life is 13.2230 hours; the decay by electron capture to tellurium-123 emits gamma radiation with a predominant energy of 159 keV. In medical applications, the radiation is detected by a gamma camera. The isotope is typically applied as iodide-123, the anionic form.
Abass Alavi is an Iranian-American physician-scientist specializing in the field of molecular imaging, most notably in the imaging modality of positron emission tomography (PET). In August 1976, he was part of the team that performed the first human PET studies of the brain and whole body using the radiotracer [18F]Fluorodeoxyglucose (FDG). Alavi holds the position of Professor of Radiology and Neurology, as well as Director of Research Education in the Department of Radiology at the University of Pennsylvania. Over a career spanning five decades, he has amassed over 2,300 publications and 60,000 citations, earning an h-index of 125 and placing his publication record in the top percentile of scientists.
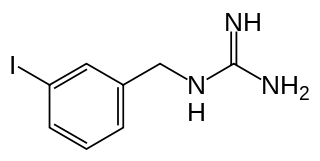
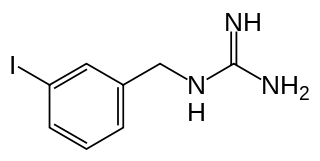
Iobenguane, or MIBG, is an aralkylguanidine analog of the adrenergic neurotransmitter norepinephrine (noradrenaline), typically used as a radiopharmaceutical. It acts as a blocking agent for adrenergic neurons. When radiolabeled, it can be used in nuclear medicinal diagnostic and therapy techniques as well as in neuroendocrine chemotherapy treatments.
Perfusion is the passage of fluid through the lymphatic system or blood vessels to an organ or a tissue. The practice of perfusion scanning is the process by which this perfusion can be observed, recorded and quantified. The term perfusion scanning encompasses a wide range of medical imaging modalities.
The American Board of Nuclear Medicine (ABNM) certifies physicians as specialists in the practice of nuclear medicine. Diplomates of the ABNM are called nuclear medicine physicians. The ABNM is one of the 24 member boards of the American Board of Medical Specialties (ABMS).

Zang-Hee Cho is a Korean neuroscientist who developed the first Ring-PET scanner and the scintillation detector BGO. More recently, Cho developed the first PET-MRI fusion molecular imaging device for neuro-molecular imaging.

Radiopharmaceuticals, or medicinal radiocompounds, are a group of pharmaceutical drugs containing radioactive isotopes. Radiopharmaceuticals can be used as diagnostic and therapeutic agents. Radiopharmaceuticals emit radiation themselves, which is different from contrast media which absorb or alter external electromagnetism or ultrasound. Radiopharmacology is the branch of pharmacology that specializes in these agents.
Preclinical or small-animal Single Photon Emission Computed Tomography (SPECT) is a radionuclide based molecular imaging modality for small laboratory animals. Although SPECT is a well-established imaging technique that is already for decades in use for clinical application, the limited resolution of clinical SPECT (~10 mm) stimulated the development of dedicated small animal SPECT systems with sub-mm resolution. Unlike in clinics, preclinical SPECT outperforms preclinical coincidence PET in terms of resolution and, at the same time, allows to perform fast dynamic imaging of animals.

Siroos Mirzaei is an Iranian specialist in Nuclear Medicine. He is Head of the Department of Nuclear Medicine of the Wilhelminen Hospital in Vienna. Mirzaei is well known for his scientific work on torture diagnostics with molecular imaging methods.
Sandip Basu is an Indian physician of Nuclear Medicine and the Head, Nuclear Medicine Academic Program at the Radiation Medicine Centre. He is also the Dean-Academic (Health-Sciences), BARC at Homi Bhabha National Institute and is known for his services and research in Nuclear Medicine, particularly on Positron emission tomography diagnostics and Targeted Radionuclide Therapy in Cancer. The Council of Scientific and Industrial Research, the apex agency of the Government of India for scientific research, awarded him the Shanti Swarup Bhatnagar Prize for Science and Technology, one of the highest Indian science awards for his contributions to Nuclear Medicine in 2012.