Microscopy is the technical field of using microscopes to view objects and areas of objects that cannot be seen with the naked eye. There are three well-known branches of microscopy: optical, electron, and scanning probe microscopy, along with the emerging field of X-ray microscopy.

Positron emission tomography (PET) is a functional imaging technique that uses radioactive substances known as radiotracers to visualize and measure changes in metabolic processes, and in other physiological activities including blood flow, regional chemical composition, and absorption. Different tracers are used for various imaging purposes, depending on the target process within the body.

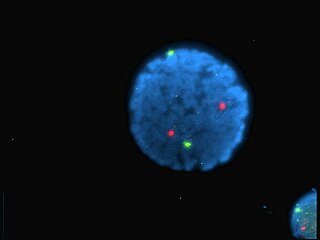
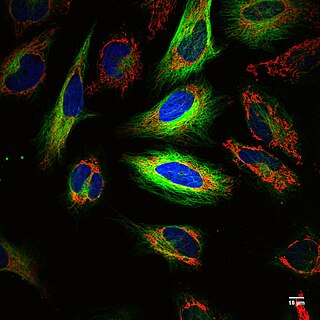
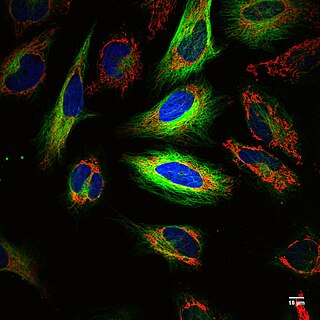
In molecular biology and biotechnology, a fluorescent tag, also known as a fluorescent label or fluorescent probe, is a molecule that is attached chemically to aid in the detection of a biomolecule such as a protein, antibody, or amino acid. Generally, fluorescent tagging, or labeling, uses a reactive derivative of a fluorescent molecule known as a fluorophore. The fluorophore selectively binds to a specific region or functional group on the target molecule and can be attached chemically or biologically. Various labeling techniques such as enzymatic labeling, protein labeling, and genetic labeling are widely utilized. Ethidium bromide, fluorescein and green fluorescent protein are common tags. The most commonly labelled molecules are antibodies, proteins, amino acids and peptides which are then used as specific probes for detection of a particular target.
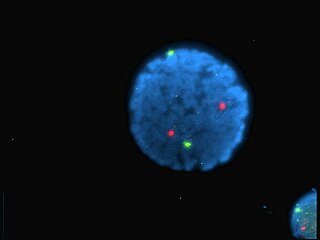
A fluorophore is a fluorescent chemical compound that can re-emit light upon light excitation. Fluorophores typically contain several combined aromatic groups, or planar or cyclic molecules with several π bonds.
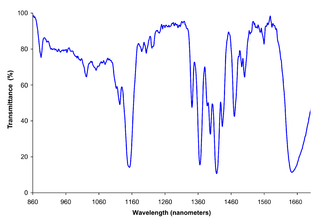
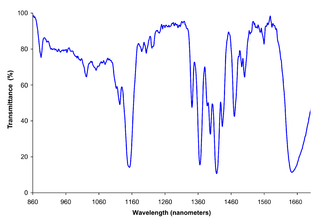
Near-infrared spectroscopy (NIRS) is a spectroscopic method that uses the near-infrared region of the electromagnetic spectrum. Typical applications include medical and physiological diagnostics and research including blood sugar, pulse oximetry, functional neuroimaging, sports medicine, elite sports training, ergonomics, rehabilitation, neonatal research, brain computer interface, urology, and neurology. There are also applications in other areas as well such as pharmaceutical, food and agrochemical quality control, atmospheric chemistry, combustion research and knowledge.

Two-photon excitation microscopy is a fluorescence imaging technique that is particularly well-suited to image scattering living tissue of up to about one millimeter in thickness. Unlike traditional fluorescence microscopy, where the excitation wavelength is shorter than the emission wavelength, two-photon excitation requires simultaneous excitation by two photons with longer wavelength than the emitted light. The laser is focused onto a specific location in the tissue and scanned across the sample to sequentially produce the image. Due to the non-linearity of two-photon excitation, mainly fluorophores in the micrometer-sized focus of the laser beam are excited, which results in the spatial resolution of the image. This contrasts with confocal microscopy, where the spatial resolution is produced by the interaction of excitation focus and the confined detection with a pinhole.
Cyanines, also referred to as tetramethylindo(di)-carbocyanines are a synthetic dye family belonging to the polymethine group. Although the name derives etymologically from terms for shades of blue, the cyanine family covers the electromagnetic spectrum from near IR to UV.

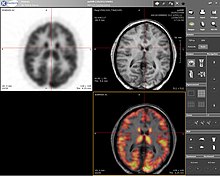
Neuroimaging is the use of quantitative (computational) techniques to study the structure and function of the central nervous system, developed as an objective way of scientifically studying the healthy human brain in a non-invasive manner. Increasingly it is also being used for quantitative research studies of brain disease and psychiatric illness. Neuroimaging is highly multidisciplinary involving neuroscience, computer science, psychology and statistics, and is not a medical specialty. Neuroimaging is sometimes confused with neuroradiology.
In medicine, a biomarker is a measurable indicator of the severity or presence of some disease state. It may be defined as a "cellular, biochemical or molecular alteration in cells, tissues or fluids that can be measured and evaluated to indicate normal biological processes, pathogenic processes, or pharmacological responses to a therapeutic intervention." More generally a biomarker is anything that can be used as an indicator of a particular disease state or some other physiological state of an organism. According to the WHO, the indicator may be chemical, physical, or biological in nature - and the measurement may be functional, physiological, biochemical, cellular, or molecular.
Functional imaging is a medical imaging technique of detecting or measuring changes in metabolism, blood flow, regional chemical composition, and absorption.

Fluorescence is used in the life sciences generally as a non-destructive way of tracking or analysing biological molecules. Some proteins or small molecules in cells are naturally fluorescent, which is called intrinsic fluorescence or autofluorescence. Alternatively, specific or general proteins, nucleic acids, lipids or small molecules can be "labelled" with an extrinsic fluorophore, a fluorescent dye which can be a small molecule, protein or quantum dot. Several techniques exist to exploit additional properties of fluorophores, such as fluorescence resonance energy transfer, where the energy is passed non-radiatively to a particular neighbouring dye, allowing proximity or protein activation to be detected; another is the change in properties, such as intensity, of certain dyes depending on their environment allowing their use in structural studies.
Preclinical imaging is the visualization of living animals for research purposes, such as drug development. Imaging modalities have long been crucial to the researcher in observing changes, either at the organ, tissue, cell, or molecular level, in animals responding to physiological or environmental changes. Imaging modalities that are non-invasive and in vivo have become especially important to study animal models longitudinally. Broadly speaking, these imaging systems can be categorized into primarily morphological/anatomical and primarily molecular imaging techniques. Techniques such as high-frequency micro-ultrasound, magnetic resonance imaging (MRI) and computed tomography (CT) are usually used for anatomical imaging, while optical imaging, positron emission tomography (PET), and single photon emission computed tomography (SPECT) are usually used for molecular visualizations.

Brain positron emission tomography is a form of positron emission tomography (PET) that is used to measure brain metabolism and the distribution of exogenous radiolabeled chemical agents throughout the brain. PET measures emissions from radioactively labeled metabolically active chemicals that have been injected into the bloodstream. The emission data from brain PET are computer-processed to produce multi-dimensional images of the distribution of the chemicals throughout the brain.
Multi-spectral optoacoustic tomography (MSOT), also known as functional photoacoustic tomography (fPAT), is an imaging technology that generates high-resolution optical images in scattering media, including biological tissues. MSOT illuminates tissue with light of transient energy, typically light pulses lasting 1-100 nanoseconds. The tissue absorbs the light pulses, and as a result undergoes thermo-elastic expansion, a phenomenon known as the optoacoustic or photoacoustic effect. This expansion gives rise to ultrasound waves (photoechoes) that are detected and formed into an image. Image formation can be done by means of hardware or computed tomography. Unlike other types of optoacoustic imaging, MSOT involves illuminating the sample with multiple wavelengths, allowing it to detect ultrasound waves emitted by different photoabsorbing molecules in the tissue, whether endogenous or exogenous. Computational techniques such as spectral unmixing deconvolute the ultrasound waves emitted by these different absorbers, allowing each emitter to be visualized separately in the target tissue. In this way, MSOT can allow visualization of hemoglobin concentration and tissue oxygenation or hypoxia. Unlike other optical imaging methods, MSOT is unaffected by photon scattering and thus can provide high-resolution optical images deep inside biological tissues.
Fluorescence guided surgery (FGS), also called fluorescence image-guided surgery, or in the specific case of tumor resection, fluorescence guided resection, is a medical imaging technique used to detect fluorescently labelled structures during surgery. Similarly to standard image-guided surgery, FGS has the purpose of guiding the surgical procedure and providing the surgeon of real time visualization of the operating field. When compared to other medical imaging modalities, FGS is cheaper and superior in terms of resolution and number of molecules detectable. As a drawback, penetration depth is usually very poor in the visible wavelengths, but it can reach up to 1–2 cm when excitation wavelengths in the near infrared are used.

18F-FMISO or fluoromisonidazole is a radiopharmaceutical used for PET imaging of hypoxia. It consists of a 2-nitroimidazole molecule labelled with the positron-emitter fluorine-18.
Preclinical or small-animal Single Photon Emission Computed Tomography (SPECT) is a radionuclide based molecular imaging modality for small laboratory animals. Although SPECT is a well-established imaging technique that is already for decades in use for clinical application, the limited resolution of clinical SPECT (~10 mm) stimulated the development of dedicated small animal SPECT systems with sub-mm resolution. Unlike in clinics, preclinical SPECT outperforms preclinical coincidence PET in terms of resolution and, at the same time, allows to perform fast dynamic imaging of animals.
Fluorescence imaging is a type of non-invasive imaging technique that can help visualize biological processes taking place in a living organism. Images can be produced from a variety of methods including: microscopy, imaging probes, and spectroscopy.
Ultrasound-switchable fluorescence (USF) imaging is a deep optics imaging technique. In last few decades, fluorescence microscopy has been highly developed to image biological samples and live tissues. However, due to light scattering, fluorescence microscopy is limited to shallow tissues. Since fluorescence is characterized by high contrast, high sensitivity, and low cost which is crucial to investigate deep tissue information, developing fluorescence imaging technique with high depth-to-resolution ratio would be promising.. Recently, ultrasound-switchable fluorescence imaging has been developed to achieve high signal-to-noise ratio (SNR) and high spatial resolution imaging without sacrificing image depth.
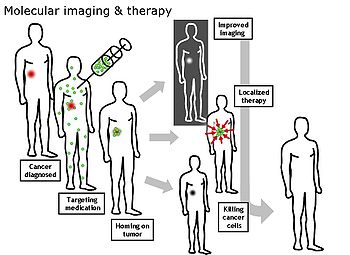
Theranostics, also known as theragnostics, is an emerging field in precision medicine that combines diagnostic and therapeutic approaches to provide the potential for personalized treatment and real-time monitoring of the effectiveness of treatments. Improvements in imaging techniques and targeted therapies are the basis of the field of theranostics. When medical imaging is coupled with the development of novel radiotracers and contrast agents, theranostics may provide opportunities for precise diagnosis and targeted therapy.