Parathyroid glands are small endocrine glands in the neck of humans and other tetrapods. Humans usually have four parathyroid glands, located on the back of the thyroid gland in variable locations. The parathyroid gland produces and secretes parathyroid hormone in response to low blood calcium, which plays a key role in regulating the amount of calcium in the blood and within the bones.

Parathyroid hormone (PTH), also called parathormone or parathyrin, is a peptide hormone secreted by the parathyroid glands that regulates the serum calcium concentration through its effects on bone, kidney, and intestine.

Calcium metabolism is the movement and regulation of calcium ions (Ca2+) in (via the gut) and out (via the gut and kidneys) of the body, and between body compartments: the blood plasma, the extracellular and intracellular fluids, and bone. Bone acts as a calcium storage center for deposits and withdrawals as needed by the blood via continual bone remodeling.
Disorders of calcium metabolism occur when the body has too little or too much calcium. The serum level of calcium is closely regulated within a fairly limited range in the human body. In a healthy physiology, extracellular calcium levels are maintained within a tight range through the actions of parathyroid hormone, vitamin D and the calcium sensing receptor. Disorders in calcium metabolism can lead to hypocalcemia, decreased plasma levels of calcium or hypercalcemia, elevated plasma calcium levels.

Parathyroid hormone-related protein (PTHrP) is a proteinaceous hormone and a member of the parathyroid hormone family secreted by mesenchymal stem cells. It is occasionally secreted by cancer cells. However, it also has normal functions in bone, teeth, vascular tissues and other tissues.

Parathyroid chief cells are one of the two cell types of the parathyroid glands, along with oxyphil cells. The chief cells are much more prevalent in the parathyroid gland than the oxyphil cells. It is perceived that oxyphil cells may be derived from chief cells at puberty, as they are not present at birth like chief cells.
Hypoparathyroidism is decreased function of the parathyroid glands with underproduction of parathyroid hormone (PTH). This can lead to low levels of calcium in the blood, often causing cramping and twitching of muscles or tetany, and several other symptoms. It is a very rare disease. The condition can be inherited, but it is also encountered after thyroid or parathyroid gland surgery, and it can be caused by immune system-related damage as well as a number of rarer causes. The diagnosis is made with blood tests, and other investigations such as genetic testing depending on the results. The primary treatment of hypoparathyroidism is calcium and vitamin D supplementation. Calcium replacement or vitamin D can ameliorate the symptoms but can increase the risk of kidney stones and chronic kidney disease. Additionally, medications such as recombinant human parathyroid hormone or teriparatide may be given by injection to replace the missing hormone.

Hyperparathyroidism is an increase in parathyroid hormone (PTH) levels in the blood. This occurs from a disorder either within the parathyroid glands or as response to external stimuli. Symptoms of hyperparathyroidism are caused by inappropriately normal or elevated blood calcium excreted from the bones and flowing into the blood stream in response to increased production of parathyroid hormone. In healthy people, when blood calcium levels are high, parathyroid hormone levels should be low. With long-standing hyperparathyroidism, the most common symptom is kidney stones. Other symptoms may include bone pain, weakness, depression, confusion, and increased urination. Both primary and secondary may result in osteoporosis.

Primary hyperparathyroidism is a medical condition where the parathyroid gland produce excess amounts of parathyroid hormone (PTH). The symptoms of the condition relate to the resulting elevated serum calcium (hypercalcemia), which can cause digestive symptoms, kidney stones, psychiatric abnormalities, and bone disease.
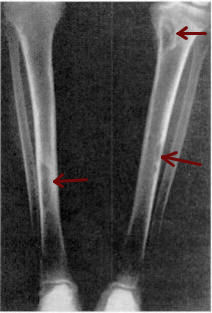
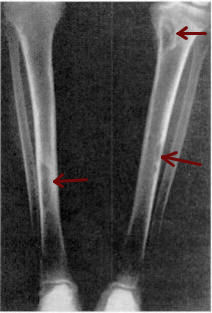
Osteitis fibrosa cystica is a skeletal disorder resulting in a loss of bone mass, a weakening of the bones as their calcified supporting structures are replaced with fibrous tissue, and the formation of cyst-like brown tumors in and around the bone. Osteitis fibrosis cystica (OFC), also known as osteitis fibrosa, osteodystrophia fibrosa, and von Recklinghausen's disease of bone, is caused by hyperparathyroidism, which is a surplus of parathyroid hormone from over-active parathyroid glands. This surplus stimulates the activity of osteoclasts, cells that break down bone, in a process known as osteoclastic bone resorption. The hyperparathyroidism can be triggered by a parathyroid adenoma, hereditary factors, parathyroid carcinoma, or renal osteodystrophy. Osteoclastic bone resorption releases minerals, including calcium, from the bone into the bloodstream, causing both elevated blood calcium levels, and the structural changes which weaken the bone. The symptoms of the disease are the consequences of both the general softening of the bones and the excess calcium in the blood, and include bone fractures, kidney stones, nausea, moth-eaten appearance in the bones, appetite loss, and weight loss.

Albright's hereditary osteodystrophy is a form of osteodystrophy, and is classified as the phenotype of pseudohypoparathyroidism type 1A; this is a condition in which the body does not respond to parathyroid hormone.
Pseudohypoparathyroidism is a rare autosomal dominant genetic condition associated primarily with resistance to the parathyroid hormone. Those with the condition have a low serum calcium and high phosphate, but the parathyroid hormone level (PTH) is inappropriately high. Its pathogenesis has been linked to dysfunctional G proteins. Pseudohypoparathyroidism is a very rare disorder, with estimated prevalence between 0.3 and 1.1 cases per 100,000 population depending on geographic location.

GNAS complex locus is a gene locus in humans. Its main product is the heterotrimeric G-protein alpha subunit Gs-α, a key component of G protein-coupled receptor-regulated adenylyl cyclase signal transduction pathways. GNAS stands for Guanine Nucleotide binding protein, Alpha Stimulating activity polypeptide.
There are two known parathyroid hormone receptors in mammals termed PTH1R and PTH2R. These receptors bind parathyroid hormone and are members of the GPCR family of transmembrane proteins.

Jansen's metaphyseal chondrodysplasia (JMC) is a disease that results from ligand-independent activation of the type 1 (PTH1R) of the parathyroid hormone receptor, due to one of three reported mutations.

Parathyroid hormone/parathyroid hormone-related peptide receptor, also known as parathyroid hormone 1 receptor (PTH1R), is a protein that in humans is encoded by the PTH1R gene. PTH1R functions as a receptor for parathyroid hormone (PTH) and for parathyroid hormone-related protein (PTHrP), also called parathyroid hormone-like hormone (PTHLH).

Parathyroid hormone 2 receptor is a protein that in humans is encoded by the PTH2R gene.
Familial hypocalciuric hypercalcemia (FHH) is an inherited condition that can cause hypercalcemia, a serum calcium level typically above 10.2 mg/dL; although uncommon. It is also known as familial benign hypocalciuric hypercalcemia (FBHH) where there is usually a family history of hypercalcemia which is mild, a urine calcium to creatinine ratio <0.01, and urine calcium <200 mg/day.

Osteoma cutis is a cutaneous condition characterized by the presence of bone within the skin in the absence of a preexisting or associated lesion. Osteoma cutis often manifests as solid, varying-sized, skin-colored subcutaneous nodules.
Archibald's sign refers to a feature in the hand characterized by a shortening of the fourth or/and fifth metacarpals when the fist is clenched.