Mechanical ventilation or assisted ventilation is the medical term for using a ventilator machine to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon dioxide. Mechanical ventilation is used for many reasons, including to protect the airway due to mechanical or neurologic cause, to ensure adequate oxygenation, or to remove excess carbon dioxide from the lungs. Various healthcare providers are involved with the use of mechanical ventilation and people who require ventilators are typically monitored in an intensive care unit.

Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by rapid onset of widespread inflammation in the lungs. Symptoms include shortness of breath (dyspnea), rapid breathing (tachypnea), and bluish skin coloration (cyanosis). For those who survive, a decreased quality of life is common.

Respiratory arrest is a serious medical condition caused by apnea or respiratory dysfunction severe enough that it will not sustain the body. Prolonged apnea refers to a patient who has stopped breathing for a long period of time. If the heart muscle contraction is intact, the condition is known as respiratory arrest. An abrupt stop of pulmonary gas exchange lasting for more than five minutes may permanently damage vital organs, especially the brain. Lack of oxygen to the brain causes loss of consciousness. Brain injury is likely if respiratory arrest goes untreated for more than three minutes, and death is almost certain if more than five minutes.
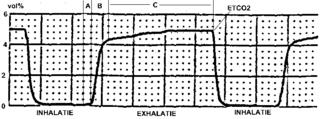
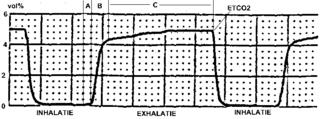
Capnography is the monitoring of the concentration or partial pressure of carbon dioxide (CO
2) in the respiratory gases. Its main development has been as a monitoring tool for use during anesthesia and intensive care. It is usually presented as a graph of CO
2 (measured in kilopascals, "kPa" or millimeters of mercury, "mmHg") plotted against time, or, less commonly, but more usefully, expired volume (known as volumetric capnography). The plot may also show the inspired CO
2, which is of interest when rebreathing systems are being used. When the measurement is taken at the end of a breath (exhaling), it is called "end tidal" CO
2 (PETCO2).

Non-invasive ventilation (NIV) is the use of breathing support administered through a face mask, nasal mask, or a helmet. Air, usually with added oxygen, is given through the mask under positive pressure; generally the amount of pressure is alternated depending on whether someone is breathing in or out. It is termed "non-invasive" because it is delivered with a mask that is tightly fitted to the face or around the head, but without a need for tracheal intubation. While there are similarities with regard to the interface, NIV is not the same as continuous positive airway pressure (CPAP), which applies a single level of positive airway pressure throughout the whole respiratory cycle; CPAP does not deliver ventilation but is occasionally used in conditions also treated with NIV.

A bag valve mask (BVM), sometimes known by the proprietary name Ambu bag or generically as a manual resuscitator or "self-inflating bag", is a hand-held device commonly used to provide positive pressure ventilation to patients who are not breathing or not breathing adequately. The device is a required part of resuscitation kits for trained professionals in out-of-hospital settings (such as ambulance crews) and is also frequently used in hospitals as part of standard equipment found on a crash cart, in emergency rooms or other critical care settings. Underscoring the frequency and prominence of BVM use in the United States, the American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiac Care recommend that "all healthcare providers should be familiar with the use of the bag-mask device." Manual resuscitators are also used within the hospital for temporary ventilation of patients dependent on mechanical ventilators when the mechanical ventilator needs to be examined for possible malfunction or when ventilator-dependent patients are transported within the hospital. Two principal types of manual resuscitators exist; one version is self-filling with air, although additional oxygen (O2) can be added but is not necessary for the device to function. The other principal type of manual resuscitator (flow-inflation) is heavily used in non-emergency applications in the operating room to ventilate patients during anesthesia induction and recovery.
Positive end-expiratory pressure (PEEP) is the pressure in the lungs above atmospheric pressure that exists at the end of expiration. The two types of PEEP are extrinsic PEEP and intrinsic PEEP. Pressure that is applied or increased during an inspiration is termed pressure support. PEEP is a therapeutic parameter set in the ventilator, or a complication of mechanical ventilation with air trapping (auto-PEEP).
High-frequency ventilation is a type of mechanical ventilation which utilizes a respiratory rate greater than four times the normal value and very small tidal volumes. High frequency ventilation is thought to reduce ventilator-associated lung injury (VALI), especially in the context of ARDS and acute lung injury. This is commonly referred to as lung protective ventilation. There are different types of high-frequency ventilation. Each type has its own unique advantages and disadvantages. The types of HFV are characterized by the delivery system and the type of exhalation phase.
Ventilator-associated lung injury (VALI) is an acute lung injury that develops during mechanical ventilation and is termed ventilator-induced lung injury (VILI) if it can be proven that the mechanical ventilation caused the acute lung injury. In contrast, ventilator-associated lung injury (VALI) exists if the cause cannot be proven. VALI is the appropriate term in most situations because it is virtually impossible to prove what actually caused the lung injury in the hospital.
Neurally adjusted ventilatory assist (NAVA) is a mode of mechanical ventilation. NAVA delivers assistance in proportion to and in synchrony with the patient's respiratory efforts, as reflected by an electrical signal. This signal represents the electrical activity of the diaphragm, the body's principal breathing muscle.
Pressure support ventilation (PSV), also known as pressure support, is a spontaneous mode of ventilation. The patient initiates every breath and the ventilator delivers support with the preset pressure value. With support from the ventilator, the patient also regulates their own respiratory rate and tidal volume.

A liquid ventilator is similar to a medical ventilator except that it should be able to ensure reliable total liquid ventilation with a breatheable liquid. Liquid ventilators are prototypes that may have been used for animal experimentations but experts recommend continued development of a liquid ventilator toward clinical applications.
Modes of mechanical ventilation are one of the most important aspects of the usage of mechanical ventilation. The mode refers to the method of inspiratory support. In general, mode selection is based on clinician familiarity and institutional preferences, since there is a paucity of evidence indicating that the mode affects clinical outcome. The most frequently used forms of volume-limited mechanical ventilation are intermittent mandatory ventilation (IMV) and continuous mandatory ventilation (CMV). There have been substantial changes in the nomenclature of mechanical ventilation over the years, but more recently it has become standardized by many respirology and pulmonology groups. Writing a mode is most proper in all capital letters with a dash between the control variable and the strategy.
Intermittent Mandatory Ventilation (IMV) refers to any mode of mechanical ventilation where a regular series of breaths are scheduled but the ventilator senses patient effort and reschedules mandatory breaths based on the calculated need of the patient. Similar to continuous mandatory ventilation in parameters set for the patients pressures and volumes but distinct in its ability to support a patient by either supporting their own effort or providing support when patient effort is not sensed. IMV is frequently paired with additional strategies to improve weaning from ventilator support or to improve cardiovascular stability in patients who may need full life support.
Inverse ratio ventilation (IRV) is not necessarily a mode of mechanical ventilation though it may be referred to as such. IRV is a strategy of ventilating the lungs in such a way that the amount of time the lungs are in inhalation is greater than the amount of time they are in exhalation, allowing for a constant inflation of the lungs, ensuring they remain "recruited". The primary goal for IRV is improved oxygenation by forcing inspiratory time to be greater than expiratory time increasing the mean airway pressure and potentially improving oxygenation. Normal I:E ratio is 5:6, so forcing the I:E to be 2:1, 3:1, 4:1, is the source of the term for the strategy.
Within the medical field of respiratory therapy, Open lung ventilation is a strategy that is utilized by several modes of mechanical ventilation to combine low tidal volume and applied PEEP to maximize recruitment of alveoli. The low tidal volume aims to minimize alveolar overdistention and the PEEP minimizes cyclic atelectasis. Working in tandem the effects from both decrease the risk of ventilator-associated lung injury.
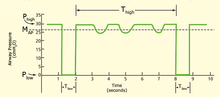
Peak inspiratory pressure (PIP) is the highest level of pressure applied to the lungs during inhalation. In mechanical ventilation the number reflects a positive pressure in centimeters of water pressure (cm H2O). In normal breathing, it may sometimes be referred to as the maximal inspiratory pressure (MIPO), which is a negative value.
There are many modes of mechanical ventilation. In medicine, mechanical ventilation is a method to mechanically assist or replace spontaneous breathing.
Dynamic hyperinflation is a phenomenon that occurs when a new breath begins before the lung has reached the static equilibrium volume. In simpler terms, this means that a new breath starts before the usual amount of air has been breathed out, leading to a build-up of air in the lungs, and causing breathing in and out to take place when the lung is nearly full.
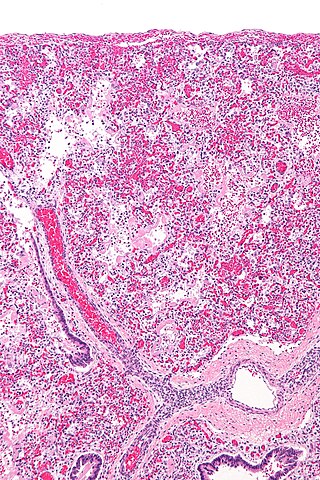
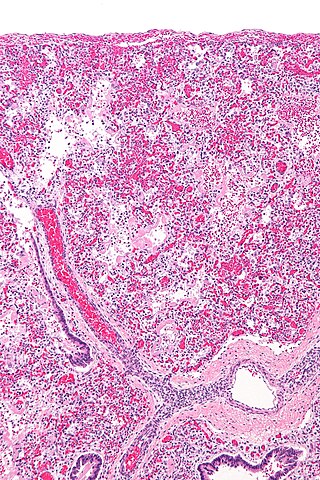
The pathophysiology of acute respiratory distress syndrome involves fluid accumulation in the lungs not explained by heart failure. It is typically provoked by an acute injury to the lungs that results in flooding of the lungs' microscopic air sacs responsible for the exchange of gases such as oxygen and carbon dioxide with capillaries in the lungs. Additional common findings in ARDS include partial collapse of the lungs (atelectasis) and low levels of oxygen in the blood (hypoxemia). The clinical syndrome is associated with pathological findings including pneumonia, eosinophilic pneumonia, cryptogenic organizing pneumonia, acute fibrinous organizing pneumonia, and diffuse alveolar damage (DAD). Of these, the pathology most commonly associated with ARDS is DAD, which is characterized by a diffuse inflammation of lung tissue. The triggering insult to the tissue usually results in an initial release of chemical signals and other inflammatory mediators secreted by local epithelial and endothelial cells.