The respiratory system is a biological system consisting of specific organs and structures used for gas exchange in animals and plants. The anatomy and physiology that make this happen varies greatly, depending on the size of the organism, the environment in which it lives and its evolutionary history. In land animals, the respiratory surface is internalized as linings of the lungs. Gas exchange in the lungs occurs in millions of small air sacs; in mammals and reptiles, these are called alveoli, and in birds, they are known as atria. These microscopic air sacs have a very rich blood supply, thus bringing the air into close contact with the blood. These air sacs communicate with the external environment via a system of airways, or hollow tubes, of which the largest is the trachea, which branches in the middle of the chest into the two main bronchi. These enter the lungs where they branch into progressively narrower secondary and tertiary bronchi that branch into numerous smaller tubes, the bronchioles. In birds, the bronchioles are termed parabronchi. It is the bronchioles, or parabronchi that generally open into the microscopic alveoli in mammals and atria in birds. Air has to be pumped from the environment into the alveoli or atria by the process of breathing which involves the muscles of respiration.
Diffusing capacity of the lung (DL) measures the transfer of gas from air in the lung, to the red blood cells in lung blood vessels. It is part of a comprehensive series of pulmonary function tests to determine the overall ability of the lung to transport gas into and out of the blood. DL, especially DLCO, is reduced in certain diseases of the lung and heart. DLCO measurement has been standardized according to a position paper by a task force of the European Respiratory and American Thoracic Societies.
Dead space is the volume of air that is inhaled that does not take part in the gas exchange, because it either remains in the conducting airways or reaches alveoli that are not perfused or poorly perfused. It means that not all the air in each breath is available for the exchange of oxygen and carbon dioxide. Mammals breathe in and out of their lungs, wasting that part of the inhalation which remains in the conducting airways where no gas exchange can occur.

Gas exchange is the physical process by which gases move passively by diffusion across a surface. For example, this surface might be the air/water interface of a water body, the surface of a gas bubble in a liquid, a gas-permeable membrane, or a biological membrane that forms the boundary between an organism and its extracellular environment.
In physiology, respiration is the movement of oxygen from the outside environment to the cells within tissues, and the removal of carbon dioxide in the opposite direction to the surrounding environment.

Hypercapnia (from the Greek hyper = "above" or "too much" and kapnos = "smoke"), also known as hypercarbia and CO2 retention, is a condition of abnormally elevated carbon dioxide (CO2) levels in the blood. Carbon dioxide is a gaseous product of the body's metabolism and is normally expelled through the lungs. Carbon dioxide may accumulate in any condition that causes hypoventilation, a reduction of alveolar ventilation (the clearance of air from the small sacs of the lung where gas exchange takes place) as well as resulting from inhalation of CO2. Inability of the lungs to clear carbon dioxide, or inhalation of elevated levels of CO2, leads to respiratory acidosis. Eventually the body compensates for the raised acidity by retaining alkali in the kidneys, a process known as "metabolic compensation".
The control of ventilation is the physiological mechanisms involved in the control of breathing, which is the movement of air into and out of the lungs. Ventilation facilitates respiration. Respiration refers to the utilization of oxygen and balancing of carbon dioxide by the body as a whole, or by individual cells in cellular respiration.

Cheyne–Stokes respiration is an abnormal pattern of breathing characterized by progressively deeper, and sometimes faster, breathing followed by a gradual decrease that results in a temporary stop in breathing called an apnea. The pattern repeats, with each cycle usually taking 30 seconds to 2 minutes. It is an oscillation of ventilation between apnea and hyperpnea with a crescendo-diminuendo pattern, and is associated with changing serum partial pressures of oxygen and carbon dioxide.
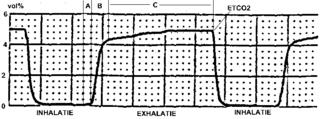
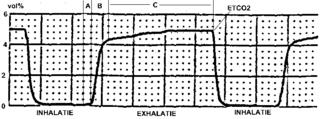
Capnography is the monitoring of the concentration or partial pressure of carbon dioxide (CO
2) in the respiratory gases. Its main development has been as a monitoring tool for use during anesthesia and intensive care. It is usually presented as a graph of CO
2 (measured in kilopascals, "kPa" or millimeters of mercury, "mmHg") plotted against time, or, less commonly, but more usefully, expired volume (known as volumetric capnography). The plot may also show the inspired CO
2, which is of interest when rebreathing systems are being used. When the measurement is taken at the end of a breath (exhaling), it is called "end tidal" CO
2 (PETCO2).

Hypoxemia is an abnormally low level of oxygen in the blood. More specifically, it is oxygen deficiency in arterial blood. Hypoxemia has many causes, and often causes hypoxia as the blood is not supplying enough oxygen to the tissues of the body.
In respiratory physiology, the ventilation/perfusion ratio is a ratio used to assess the efficiency and adequacy of the ventilation-perfusion coupling and thus the matching of two variables:
The factors that determine the values for alveolar pO2 and pCO2 are:
The Alveolar–arterial gradient, is a measure of the difference between the alveolar concentration (A) of oxygen and the arterial (a) concentration of oxygen. It is a useful parameter for narrowing the differential diagnosis of hypoxemia.

The breathing performance of regulators is a measure of the ability of a breathing gas regulator to meet the demands placed on it at varying ambient pressures and temperatures, and under varying breathing loads, for the range of breathing gases it may be expected to deliver. Performance is an important factor in design and selection of breathing regulators for any application, but particularly for underwater diving, as the range of ambient operating pressures and temperatures, and variety of breathing gases is broader in this application. A diving regulator is a device that reduces the high pressure in a diving cylinder or surface supply hose to the same pressure as the diver's surroundings. It is desirable that breathing from a regulator requires low effort even when supplying large amounts of breathing gas as this is commonly the limiting factor for underwater exertion, and can be critical during diving emergencies. It is also preferable that the gas is delivered smoothly without any sudden changes in resistance while inhaling or exhaling, and that the regulator does not lock up and either fail to supply gas or free-flow. Although these factors may be judged subjectively, it is convenient to have standards by which the many different types and manufactures of regulators may be objectively compared.
The Bohr equation, named after Danish physician Christian Bohr (1855–1911), describes the amount of physiological dead space in a person's lungs. This is given as a ratio of dead space to tidal volume. It differs from anatomical dead space as measured by Fowler's method as it includes alveolar dead space.

Breathing is the rhythmical process of moving air into (inhalation) and out of (exhalation) the lungs to facilitate gas exchange with the internal environment, mostly to flush out carbon dioxide and bring in oxygen.

Indirect calorimetry calculates heat that living organisms produce by measuring either their production of carbon dioxide and nitrogen waste, or from their consumption of oxygen. Indirect calorimetry estimates the type and rate of substrate utilization and energy metabolism in vivo starting from gas exchange measurements. This technique provides unique information, is noninvasive, and can be advantageously combined with other experimental methods to investigate numerous aspects of nutrient assimilation, thermogenesis, the energetics of physical exercise, and the pathogenesis of metabolic diseases.
Work of breathing (WOB) is the energy expended to inhale and exhale a breathing gas. It is usually expressed as work per unit volume, for example, joules/litre, or as a work rate (power), such as joules/min or equivalent units, as it is not particularly useful without a reference to volume or time. It can be calculated in terms of the pulmonary pressure multiplied by the change in pulmonary volume, or in terms of the oxygen consumption attributable to breathing.
Human physiology of underwater diving is the physiological influences of the underwater environment on the human diver, and adaptations to operating underwater, both during breath-hold dives and while breathing at ambient pressure from a suitable breathing gas supply. It, therefore, includes the range of physiological effects generally limited to human ambient pressure divers either freediving or using underwater breathing apparatus. Several factors influence the diver, including immersion, exposure to the water, the limitations of breath-hold endurance, variations in ambient pressure, the effects of breathing gases at raised ambient pressure, effects caused by the use of breathing apparatus, and sensory impairment. All of these may affect diver performance and safety.

Ventilation–perfusion coupling is the relationship between ventilation and perfusion processes, which take place in the respiratory system and the cardiovascular system. Ventilation is the movement of gas during breathing, and perfusion is the process of pulmonary blood circulation, which delivers oxygen to body tissues. Anatomically, the lung structure, alveolar organization, and alveolar capillaries contribute to the physiological mechanism of ventilation and perfusion. Ventilation–perfusion coupling maintains a constant ventilation/perfusion ratio near 0.8 on average, while the regional variation exists within the lungs due to gravity. When the ratio gets above or below 0.8, it is considered abnormal ventilation-perfusion coupling, also known as a ventilation–perfusion mismatch. Lung diseases, cardiac shunts, and smoking can cause a ventilation-perfusion mismatch that results in significant symptoms and diseases, which can be treated through treatments like bronchodilators and oxygen therapy.