Cerebrospinal fluid (CSF) is a clear, colorless body fluid found in the brain and spinal cord. It is produced by specialised ependymal cells in the choroid plexuses of the ventricles of the brain, and absorbed in the arachnoid granulations. There is about 125 mL of CSF at any one time, and about 500 mL is generated every day. CSF acts as a cushion or buffer, providing basic mechanical and immunological protection to the brain inside the skull. CSF also serves a vital function in the cerebral autoregulation of cerebral blood flow.

Hypoxia is a condition in which the body or a region of the body is deprived of adequate oxygen supply at the tissue level. Hypoxia may be classified as either generalized, affecting the whole body, or local, affecting a region of the body. Although hypoxia is often a pathological condition, variations in arterial oxygen concentrations can be part of the normal physiology, for example, during hypoventilation training or strenuous physical exercise.
A chemoreceptor, also known as chemosensor, is a specialized sensory receptor cell which transduces a chemical substance to generate a biological signal. This signal may be in the form of an action potential, if the chemoreceptor is a neuron, or in the form of a neurotransmitter that can activate a nerve fiber if the chemoreceptor is a specialized cell, such as taste receptors, or an internal peripheral chemoreceptor, such as the carotid bodies. In physiology, a chemoreceptor detects changes in the normal environment, such as an increase in blood levels of carbon dioxide (hypercapnia) or a decrease in blood levels of oxygen (hypoxia), and transmits that information to the central nervous system which engages body responses to restore homeostasis.
Acidosis is a process causing increased acidity in the blood and other body tissues. If not further qualified, it usually refers to acidity of the blood plasma.

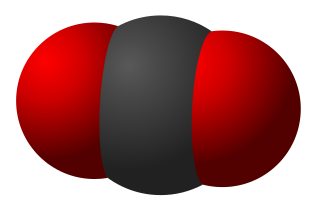
Hypercapnia (from the Greek hyper = "above" or "too much" and kapnos = "smoke"), also known as hypercarbia and CO2 retention, is a condition of abnormally elevated carbon dioxide (CO2) levels in the blood. Carbon dioxide is a gaseous product of the body's metabolism and is normally expelled through the lungs. Carbon dioxide may accumulate in any condition that causes hypoventilation, a reduction of alveolar ventilation (the clearance of air from the small sacs of the lung where gas exchange takes place). Inability of the lungs to clear carbon dioxide leads to respiratory acidosis. Eventually the body compensates for the raised acidity by retaining alkali in the kidneys, a process known as "metabolic compensation".

Intracranial pressure (ICP) is the pressure exerted by fluids such as cerebrospinal fluid (CSF) inside the skull and on the brain tissue. ICP is measured in millimeters of mercury (mmHg) and, at rest, is normally 7–15 mmHg for a supine adult. The body has various mechanisms by which it keeps the ICP stable, with CSF pressures varying by about 1 mmHg in normal adults through shifts in production and absorption of CSF.
The control of ventilation refers to the physiological mechanisms involved in the control of breathing, which is the movement of air into and out of the lungs. Ventilation facilitates respiration. Respiration refers to the utilization of oxygen and balancing of carbon dioxide by the body as a whole, or by individual cells in cellular respiration.

The carotid body is a small cluster of chemoreceptor cells, and supporting sustentacular cells. The carotid body is located in the adventitia, in the bifurcation (fork) of the common carotid artery, which runs along both sides of the neck.
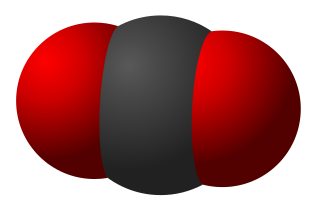
Hypocapnia or hypocapnea, also known as hypocarbia, sometimes incorrectly called acapnia, is a state of reduced carbon dioxide in the blood. Hypocapnia usually results from deep or rapid breathing, known as hyperventilation.
Cushing reflex is a physiological nervous system response to increased intracranial pressure (ICP) that results in Cushing's triad of increased blood pressure, irregular breathing, and bradycardia. It is usually seen in the terminal stages of acute head injury and may indicate imminent brain herniation. It can also be seen after the intravenous administration of epinephrine and similar drugs. It was first described in detail by American neurosurgeon Harvey Cushing in 1901.

Respiratory acidosis is a state in which decreased ventilation (hypoventilation) increases the concentration of carbon dioxide in the blood and decreases the blood's pH.

Glomus cells are the cell type mainly located in the carotid bodies and aortic bodies. Glomus type I cells are peripheral chemoreceptors which sense the oxygen, carbon dioxide and pH levels of the blood. When there is a decrease in the blood's pH, a decrease in oxygen (pO2), or an increase in carbon dioxide (pCO2), the carotid bodies and the aortic bodies signal the dorsal respiratory group in the medulla oblongata to increase the volume and rate of breathing. The glomus cells have a high metabolic rate and good blood perfusion and thus are sensitive to changes in arterial blood gas tension. Glomus type II cells are sustentacular cells having a similar supportive function to glial cells.
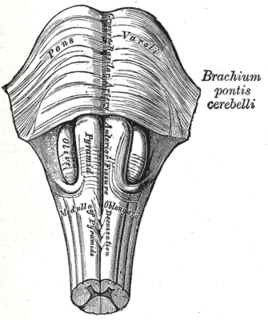
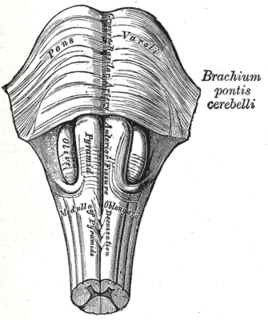
Central neurogenic hyperventilation (CNH) is an abnormal pattern of breathing characterized by deep and rapid breaths at a rate of at least 25 breaths per minute. Increasing irregularity of this respiratory rate generally is a sign that the patient will enter into coma. CNH is unrelated to other forms of hyperventilation, like Kussmaul's respirations. CNH is the human body's response to reduced carbon dioxide levels in the blood. This reduction in carbon dioxide is caused by contraction of cranial arteries from damage caused by lesions in the brain stem. However, the mechanism by which CNH arises as a result from these lesions is still very poorly understood. Current research has yet to provide an effective means of treatment for the rare number of patients who are diagnosed with this condition.
Hypoxemia is an abnormally low level of oxygen in the blood. More specifically, it is oxygen deficiency in arterial blood. Hypoxemia has many causes, and often causes hypoxia as the blood is not supplying enough oxygen to the tissues of the body.

Metabolic alkalosis is a metabolic condition in which the pH of tissue is elevated beyond the normal range (7.35–7.45). This is the result of decreased hydrogen ion concentration, leading to increased bicarbonate, or alternatively a direct result of increased bicarbonate concentrations. The condition typically cannot last long if the kidneys are functioning properly.
Acid–base homeostasis is the homeostatic regulation of the pH of the body's extracellular fluid (ECF). The proper balance between the acids and bases in the ECF is crucial for the normal physiology of the body, and cellular metabolism. The pH of the intracellular fluid and the extracellular fluid need to be maintained at a constant level.
Peripheral chemoreceptors are so named because they are sensory extensions of the peripheral nervous system into blood vessels where they detect changes in chemical concentrations. As transducers of patterns of variability in the surrounding environment, carotid and aortic bodies count as chemosensors in a similar way as taste buds and photoreceptors. However, because carotid and aortic bodies detect variation within the body’s internal organs, they are considered interoceptors. Taste buds, olfactory bulbs, photoreceptors, and other receptors associated with the five traditional sensory modalities, by contrast, are exteroceptors in that they respond to stimuli outside the body. The body also contains proprioceptors, which respond to the amount of stretch within the organ, usually muscle, that they occupy.
The vasomotor center (VMC) is a portion of the medulla oblongata. Together with the cardiovascular center and respiratory center, it regulates blood pressure. It also has a more minor role in other homeostatic processes. Upon increase in carbon dioxide level at central chemoreceptors, it stimulates the sympathetic system to constrict vessels. This is opposite to carbon dioxide in tissues causing vasodilatation, especially in the brain. Cranial nerves IX and X both feed into the vasomotor centre and are themselves involved in the regulation of blood pressure.

Breathing is the process of moving air into and out of the lungs to facilitate gas exchange with the internal environment, mostly to bring in oxygen and flush out carbon dioxide.

The slice preparation or brain slice is a laboratory technique in electrophysiology that allows the study of a synapse or neural circuit in isolation from the rest of the brain, in controlled physiological conditions. Brain tissue is initially sliced via a tissue slicer then immersed in artificial cerebrospinal fluid (aCSF) for stimulation and/or recording. The technique allows for greater experimental control, through elimination of the effects of the rest of the brain on the circuit of interest, careful control of the physiological conditions through perfusion of substrates through the incubation fluid, to precise manipulation of neurotransmitter activity through perfusion of agonists and antagonists. However, the increase in control comes with a decrease in the ease with which the results can be applied to the whole neural system.