Related Research Articles

Hypoxia is a condition in which the body or a region of the body is deprived of adequate oxygen supply at the tissue level. Hypoxia may be classified as either generalized, affecting the whole body, or local, affecting a region of the body. Although hypoxia is often a pathological condition, variations in arterial oxygen concentrations can be part of the normal physiology, for example, during strenuous physical exercise.

Meconium aspiration syndrome (MAS) also known as neonatal aspiration of meconium is a medical condition affecting newborn infants. It describes the spectrum of disorders and pathophysiology of newborns born in meconium-stained amniotic fluid (MSAF) and have meconium within their lungs. Therefore, MAS has a wide range of severity depending on what conditions and complications develop after parturition. Furthermore, the pathophysiology of MAS is multifactorial and extremely complex which is why it is the leading cause of morbidity and mortality in term infants.

The respiratory system is a biological system consisting of specific organs and structures used for gas exchange in animals and plants. The anatomy and physiology that make this happen varies greatly, depending on the size of the organism, the environment in which it lives and its evolutionary history. In land animals, the respiratory surface is internalized as linings of the lungs. Gas exchange in the lungs occurs in millions of small air sacs; in mammals and reptiles, these are called alveoli, and in birds, they are known as atria. These microscopic air sacs have a very rich blood supply, thus bringing the air into close contact with the blood. These air sacs communicate with the external environment via a system of airways, or hollow tubes, of which the largest is the trachea, which branches in the middle of the chest into the two main bronchi. These enter the lungs where they branch into progressively narrower secondary and tertiary bronchi that branch into numerous smaller tubes, the bronchioles. In birds, the bronchioles are termed parabronchi. It is the bronchioles, or parabronchi that generally open into the microscopic alveoli in mammals and atria in birds. Air has to be pumped from the environment into the alveoli or atria by the process of breathing which involves the muscles of respiration.
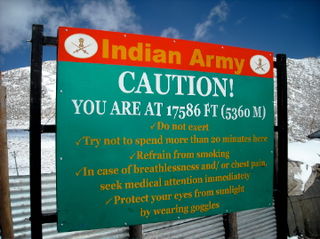
Altitude sickness, the mildest form being acute mountain sickness (AMS), is a harmful effect of high altitude, caused by rapid exposure to low amounts of oxygen at high elevation. People can respond to high altitude in different ways. Symptoms may include headaches, vomiting, tiredness, confusion, trouble sleeping, and dizziness. Acute mountain sickness can progress to high-altitude pulmonary edema (HAPE) with associated shortness of breath or high-altitude cerebral edema (HACE) with associated confusion. Chronic mountain sickness may occur after long-term exposure to high altitude.
Dead space is the volume of air that is inhaled that does not take part in the gas exchange, because it either remains in the conducting airways or reaches alveoli that are not perfused or poorly perfused. It means that not all the air in each breath is available for the exchange of oxygen and carbon dioxide. Mammals breathe in and out of their lungs, wasting that part of the inhalation which remains in the conducting airways where no gas exchange can occur.

Pulmonary edema, also known as pulmonary congestion, is excessive fluid accumulation in the tissue or air spaces of the lungs. This leads to impaired gas exchange, most often leading to shortness of breath (dyspnea) which can progress to hypoxemia and respiratory failure. Pulmonary edema has multiple causes and is traditionally classified as cardiogenic or noncardiogenic.

The diving reflex, also known as the diving response and mammalian diving reflex, is a set of physiological responses to immersion that overrides the basic homeostatic reflexes, and is found in all air-breathing vertebrates studied to date. It optimizes respiration by preferentially distributing oxygen stores to the heart and brain, enabling submersion for an extended time.
Vascular resistance is the resistance that must be overcome for blood to flow through the circulatory system. The resistance offered by the systemic circulation is known as the systemic vascular resistance (SVR) or may sometimes be called by the older term total peripheral resistance (TPR), while the resistance offered by the pulmonary circulation is known as the pulmonary vascular resistance (PVR). Systemic vascular resistance is used in calculations of blood pressure, blood flow, and cardiac function. Vasoconstriction increases SVR, whereas vasodilation decreases SVR.

Pulmonary hypertension is a condition of increased blood pressure in the arteries of the lungs. Symptoms include shortness of breath, fainting, tiredness, chest pain, swelling of the legs, and a fast heartbeat. The condition may make it difficult to exercise. Onset is typically gradual. According to the definition at the 6th World Symposium of Pulmonary Hypertension in 2018, a patient is deemed to have pulmonary hypertension if the pulmonary mean arterial pressure is greater than 20mmHg at rest, revised down from a purely arbitrary 25mmHg, and pulmonary vascular resistance (PVR) greater than 3 Wood units.

Generalized hypoxia is a medical condition in which the tissues of the body are deprived of the necessary levels of oxygen due to an insufficient supply of oxygen, which may be due to the composition or pressure of the breathing gas, decreased lung ventilation, or respiratory disease, any of which may cause a lower than normal oxygen content in the arterial blood, and consequently a reduced supply of oxygen to all tissues perfused by the arterial blood. This usage is in contradistinction to localized hypoxia, in which only an associated group of tissues, usually with a common blood supply, are affected, usually due to an insufficient or reduced blood supply to those tissues. Generalized hypoxia is also used as a synonym for hypoxic hypoxia This is not to be confused with hypoxemia, which refers to low levels of oxygen in the blood, although the two conditions often occur simultaneously, since a decrease in blood oxygen typically corresponds to a decrease in oxygen in the surrounding tissue. However, hypoxia may be present without hypoxemia, and vice versa, as in the case of infarction. Several other classes of medical hypoxia exist.

High-altitude pulmonary edema (HAPE) is a life-threatening form of non-cardiogenic pulmonary edema that occurs in otherwise healthy people at altitudes typically above 2,500 meters (8,200 ft). However, cases have also been reported between 1,500–2,500 metres or 4,900–8,200 feet in more vulnerable subjects.
Hyperoxia occurs when cells, tissues and organs are exposed to an excess supply of oxygen (O2) or higher than normal partial pressure of oxygen.

Hypoxemia is an abnormally low level of oxygen in the blood. More specifically, it is oxygen deficiency in arterial blood. Hypoxemia has many causes, and often causes hypoxia as the blood is not supplying enough oxygen to the tissues of the body.
Aerospace physiology is the study of the effects of high altitudes on the body, such as different pressures and levels of oxygen. At different altitudes the body may react in different ways, provoking more cardiac output, and producing more erythrocytes. These changes cause more energy waste in the body, causing muscle fatigue, but this varies depending on the level of the altitude.
A pulmonary shunt is the passage of deoxygenated blood from the right side of the heart to the left without participation in gas exchange in the pulmonary capillaries. It is a pathological condition that results when the alveoli of parts of the lungs are perfused with blood as normal, but ventilation fails to supply the perfused region. In other words, the ventilation/perfusion ratio of those areas is zero.

The effects of high altitude on humans are mostly the consequences of reduced partial pressure of oxygen in the atmosphere. The medical problems that are direct consequence of high altitude are caused by the low inspired partial pressure of oxygen, which is caused by the reduced atmospheric pressure, and the constant gas fraction of oxygen in atmospheric air over the range in which humans can survive. The other major effect of altitude is due to lower ambient temperature.

Transient receptor potential cation channel, subfamily C, member 6 or Transient receptor potential canonical 6, also known as TRPC6, is a human gene encoding a protein of the same name. TRPC6 is a transient receptor potential channel of the classical TRPC subfamily.
Juxtacapillary receptors, J-receptors, or pulmonary C-fiber receptors are sensory nerve endings located within the alveolar walls in juxtaposition to the pulmonary capillaries of the lung, and are innervated by fibers of the vagus nerve. Although their functional role is unclear, J-receptors respond to events such as pulmonary edema, pulmonary emboli, pneumonia, congestive heart failure and barotrauma, which cause a decrease in oxygenation and thus lead to an increase in respiration. They may be also stimulated by hyperinflation of the lung as well as intravenous or intracardiac administration of chemicals such as capsaicin. The stimulation of the J-receptors causes a reflex increase in breathing rate, and is also thought to be involved in the sensation of dyspnea, the subjective sensation of difficulty breathing. The reflex response that is produced is apnea followed by rapid breathing, bradycardia, and hypotension. The physiologic role of this reflex is uncertain, but it probably occurs in pathologic states such as pulmonary congestion or embolization. These receptors were discovered by Autar Paintal.
Hypoxic ventilatory response (HVR) is the increase in ventilation induced by hypoxia that allows the body to take in and transport lower concentrations of oxygen at higher rates. It is initially elevated in lowlanders who travel to high altitude, but reduces significantly over time as people acclimatize. In biological anthropology, HVR also refers to human adaptation to environmental stresses resulting from high altitude.
Swimming induced pulmonary edema (SIPE), also known as immersion pulmonary edema, is a life threatening condition that occurs when fluids from the blood leak abnormally from the small vessels of the lung (pulmonary capillaries) into the airspaces (alveoli).
References
- ↑ Silverthorn, D.U. (2016). "Chapter 14-15". Human physiology (7th ed.). New York: Pearson Education. p. 544.
- ↑ Sylvester, J. T.; Shimoda, Larissa A.; Aaronson, Philip I.; Ward, Jeremy P. T. (2012-01-01). "Hypoxic pulmonary vasoconstriction". Physiological Reviews. 92 (1): 367–520. doi:10.1152/physrev.00041.2010. ISSN 1522-1210. PMC 9469196 . PMID 22298659. S2CID 78887723.
- ↑ Post, J. M.; Hume, J. R.; Archer, S. L.; Weir, E. K. (1992-04-01). "Direct role for potassium channel inhibition in hypoxic pulmonary vasoconstriction". The American Journal of Physiology. 262 (4 Pt 1): C882–890. doi:10.1152/ajpcell.1992.262.4.C882. ISSN 0002-9513. PMID 1566816.
- ↑ Yuan, X. J.; Goldman, W. F.; Tod, M. L.; Rubin, L. J.; Blaustein, M. P. (1993-02-01). "Hypoxia reduces potassium currents in cultured rat pulmonary but not mesenteric arterial myocytes". The American Journal of Physiology. 264 (2 Pt 1): L116–123. doi:10.1152/ajplung.1993.264.2.L116. ISSN 0002-9513. PMID 8447425. S2CID 31223667.
- ↑ Weissmann, Norbert; Dietrich, Alexander; Fuchs, Beate; Kalwa, Hermann; Ay, Mahmut; Dumitrascu, Rio; Olschewski, Andrea; Storch, Ursula; Mederos y Schnitzler, Michael (2006-12-12). "Classical transient receptor potential channel 6 (TRPC6) is essential for hypoxic pulmonary vasoconstriction and alveolar gas exchange". Proceedings of the National Academy of Sciences of the United States of America. 103 (50): 19093–19098. Bibcode:2006PNAS..10319093W. doi: 10.1073/pnas.0606728103 . ISSN 0027-8424. PMC 1748182 . PMID 17142322.
- ↑ Goldenberg, Neil M.; Wang, Liming; Ranke, Hannes; Liedtke, Wolfgang; Tabuchi, Arata; Kuebler, Wolfgang M. (2015-06-01). "TRPV4 Is Required for Hypoxic Pulmonary Vasoconstriction". Anesthesiology. 122 (6): 1338–1348. doi:10.1097/ALN.0000000000000647. ISSN 1528-1175. PMID 25815455. S2CID 24364626.
- ↑ Wang, Liming; Yin, Jun; Nickles, Hannah T.; Ranke, Hannes; Tabuchi, Arata; Hoffmann, Julia; Tabeling, Christoph; Barbosa-Sicard, Eduardo; Chanson, Marc; Kwak, Brenda R.; Shin, Heesup S.; Wu, Songwei; Isakson, Brant E.; Witzenrath, Martin; de Wit, Cor; Fleming, Ingrid; Kuppe, Hermann; Kuebler, Wolfgang M. (2012-11-01). "Hypoxic pulmonary vasoconstriction requires connexin 40-mediated endothelial signal conduction". The Journal of Clinical Investigation. 122 (11): 4218–4230. doi:10.1172/JCI59176. ISSN 1558-8238. PMC 3484430 . PMID 23093775.
- ↑ Lauweryns, Joseph M.; Cokelaere, Marnix; Theunynck, Paul (1973). "Serotonin Producing Neuroepithelial Bodies in Rabbit Respiratory Mucosa". Science. 180 (4084): 410–413. doi:10.1126/science.180.4084.410. ISSN 0036-8075.
- ↑ Swenson, Erik R. (24 Jun 2013). "Hypoxic Pulmonary Vasoconstriction". High Altitude Medicine & Biology. 14 (2): 101–110. doi:10.1089/ham.2013.1010. PMID 23795729.
- Von Euler US, Liljestrand G (1946). "Observations on the pulmonary arterial blood pressure in the cat". Acta Physiol. Scand. 12 (4): 301–320. doi:10.1111/j.1748-1716.1946.tb00389.x.
- Völkel N, Duschek W, Kaukel E, Beier W, Siemssen S, Sill V (1975). "Histamine-an important mediator for the Euler-Liljestrand mechanism?". Pneumonologie. Pneumonology. 152 (1–3): 113–21. doi:10.1007/BF02101579. PMID 171630. S2CID 27167180.
- Porcelli RJ, Viau A, Demeny M, Naftchi NE, Bergofsky EH (1977). "Relation between hypoxic pulmonary vasoconstriction, its humoral mediators and alpha-beta adrenergic receptors". Chest. 71 (2 suppl): 249–251. doi:10.1378/chest.71.2_Supplement.249. PMID 12924.