Equation
- [1]
- : Fraction of inspired oxygen, in percent;
- : Mean airway pressure, in mmHg;
- : Partial pressure of oxygen in arterial blood, in mmHg.
The oxygenation index is a calculation used in intensive care medicine to measure the fraction of inspired oxygen (FiO2) and its usage within the body.
A lower oxygenation index is better - this can be inferred by the equation itself. As the oxygenation of a person improves, they will be able to achieve a higher PaO2 at a lower FiO2. This would be reflected on the formula as a decrease in the numerator or an increase in the denominator - thus lowering the OI. Typically an OI threshold is set for when a neonate should be placed on ECMO, for example >40.

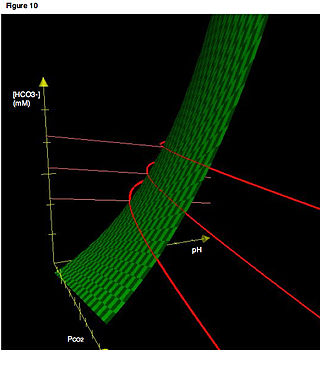
In a mixture of gases, each constituent gas has a partial pressure which is the notional pressure of that constituent gas as if it alone occupied the entire volume of the original mixture at the same temperature. The total pressure of an ideal gas mixture is the sum of the partial pressures of the gases in the mixture.
In chemistry and thermodynamics, the standard enthalpy of formation or standard heat of formation of a compound is the change of enthalpy during the formation of 1 mole of the substance from its constituent elements in their reference state, with all substances in their standard states. The standard pressure value p⦵ = 105 Pa(= 100 kPa = 1 bar) is recommended by IUPAC, although prior to 1982 the value 1.00 atm (101.325 kPa) was used. There is no standard temperature. Its symbol is ΔfH⦵. The superscript Plimsoll on this symbol indicates that the process has occurred under standard conditions at the specified temperature (usually 25 °C or 298.15 K).

Respiratory failure results from inadequate gas exchange by the respiratory system, meaning that the arterial oxygen, carbon dioxide, or both cannot be kept at normal levels. A drop in the oxygen carried in the blood is known as hypoxemia; a rise in arterial carbon dioxide levels is called hypercapnia. Respiratory failure is classified as either Type 1 or Type 2, based on whether there is a high carbon dioxide level, and can be acute or chronic. In clinical trials, the definition of respiratory failure usually includes increased respiratory rate, abnormal blood gases, and evidence of increased work of breathing. Respiratory failure causes an altered state of consciousness due to ischemia in the brain.
An arterial blood gas (ABG) test, or arterial blood gas analysis (ABGA) measures the amounts of arterial gases, such as oxygen and carbon dioxide. An ABG test requires that a small volume of blood be drawn from the radial artery with a syringe and a thin needle, but sometimes the femoral artery in the groin or another site is used. The blood can also be drawn from an arterial catheter.

Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by rapid onset of widespread inflammation in the lungs. Symptoms include shortness of breath (dyspnea), rapid breathing (tachypnea), and bluish skin coloration (cyanosis). For those who survive, a decreased quality of life is common.
The Fick principle states that blood flow to an organ can be calculated using a marker substance if the following information is known:
Air–fuel ratio (AFR) is the mass ratio of air to a solid, liquid, or gaseous fuel present in a combustion process. The combustion may take place in a controlled manner such as in an internal combustion engine or industrial furnace, or may result in an explosion ,The air–fuel ratio determines whether a mixture is combustible at all, how much energy is being released, and how much unwanted pollutants are produced in the reaction. Typically a range of fuel to air ratios exists, outside of which ignition will not occur. These are known as the lower and upper explosive limits.
Hyperoxia occurs when cells, tissues and organs are exposed to an excess supply of oxygen (O2) or higher than normal partial pressure of oxygen.
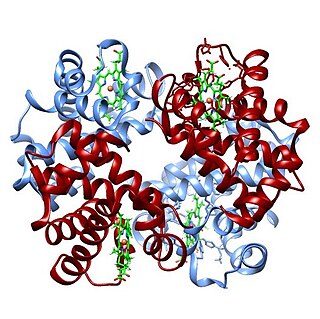
The oxygen–hemoglobin dissociation curve, also called the oxyhemoglobin dissociation curve or oxygen dissociation curve (ODC), is a curve that plots the proportion of hemoglobin in its saturated (oxygen-laden) form on the vertical axis against the prevailing oxygen tension on the horizontal axis. This curve is an important tool for understanding how our blood carries and releases oxygen. Specifically, the oxyhemoglobin dissociation curve relates oxygen saturation (SO2) and partial pressure of oxygen in the blood (PO2), and is determined by what is called "hemoglobin affinity for oxygen"; that is, how readily hemoglobin acquires and releases oxygen molecules into the fluid that surrounds it.
A pulmonary shunt is the passage of deoxygenated blood from the right side of the heart to the left without participation in gas exchange in the pulmonary capillaries. It is a pathological condition that results when the alveoli of parts of the lungs are perfused with blood as normal, but ventilation fails to supply the perfused region. In other words, the ventilation/perfusion ratio of those areas is zero.
The alveolar gas equation is the method for calculating partial pressure of alveolar oxygen. The equation is used in assessing if the lungs are properly transferring oxygen into the blood. The alveolar air equation is not widely used in clinical medicine, probably because of the complicated appearance of its classic forms. The partial pressure of oxygen in the pulmonary alveoli is required to calculate both the alveolar-arterial gradient of oxygen and the amount of right-to-left cardiac shunt, which are both clinically useful quantities. However, it is not practical to take a sample of gas from the alveoli in order to directly measure the partial pressure of oxygen. The alveolar gas equation allows the calculation of the alveolar partial pressure of oxygen from data that is practically measurable. It was first characterized in 1946.
The multiple inert gas elimination technique (MIGET) is a medical technique used mainly in pulmonology that involves measuring the concentrations of various infused, inert gases in mixed venous blood, arterial blood, and expired gas of a subject. The technique quantifies true shunt, physiological dead space ventilation, ventilation versus blood flow ratios, and diffusion limitation.
The Alveolar–arterial gradient, is a measure of the difference between the alveolar concentration (A) of oxygen and the arterial (a) concentration of oxygen. It is a useful parameter for narrowing the differential diagnosis of hypoxemia.
The Shunt equation quantifies the extent to which venous blood bypasses oxygenation in the capillaries of the lung. “Shunt” and “dead space“ are terms used to describe conditions where either blood flow or ventilation do not interact with each other in the lung, as they should for efficient gas exchange to take place. These terms can also be used to describe areas or effects where blood flow and ventilation are not properly matched, though both may be present to varying degrees. Some references refer to “shunt-effect” or “dead space-effect” to designate the ventilation/perfusion mismatch states that are less extreme than absolute shunt or dead space.
The Hypoxic Training index (HTi) provides an objective measure of the hypoxic stress delivered during the Intermittent Hypoxic Training (IHT) session, compared to simple recording the inhaled fraction of oxygen (FiO2). HTi provides a figure (index) of dosage received by the individual at the end of the session. Knowledge of HTi can therefore be used to alter the training regime for different individuals, compensating for individual variability, and can be used in scientific studies to ensure that subject exposure was correctly controlled.

Oxygen saturation is the fraction of oxygen-saturated haemoglobin relative to total haemoglobin in the blood. The human body requires and regulates a very precise and specific balance of oxygen in the blood. Normal arterial blood oxygen saturation levels in humans are 96–100 percent. If the level is below 90 percent, it is considered low and called hypoxemia. Arterial blood oxygen levels below 80 percent may compromise organ function, such as the brain and heart, and should be promptly addressed. Continued low oxygen levels may lead to respiratory or cardiac arrest. Oxygen therapy may be used to assist in raising blood oxygen levels. Oxygenation occurs when oxygen molecules enter the tissues of the body. For example, blood is oxygenated in the lungs, where oxygen molecules travel from the air and into the blood. Oxygenation is commonly used to refer to medical oxygen saturation.

In thermodynamics, the volume of a system is an important extensive parameter for describing its thermodynamic state. The specific volume, an intensive property, is the system's volume per unit mass. Volume is a function of state and is interdependent with other thermodynamic properties such as pressure and temperature. For example, volume is related to the pressure and temperature of an ideal gas by the ideal gas law. The physical region covered by a system may or may not coincide with a control volume used to analyze the system.
The Horowitz index or Horovitz index is a ratio used to assess lung function in patients, particularly those on ventilators. Overall, it is useful for evaluating the extent of damage to the lungs. The simple abbreviation as oxygenation can lead to confusion with other conceptualizations of oxygenation index.
Fraction of inspired oxygen (FIO2), correctly denoted with a capital I, is the molar or volumetric fraction of oxygen in the inhaled gas. Medical patients experiencing difficulty breathing are provided with oxygen-enriched air, which means a higher-than-atmospheric FIO2. Natural air includes 21% oxygen, which is equivalent to FIO2 of 0.21. Oxygen-enriched air has a higher FIO2 than 0.21; up to 1.00 which means 100% oxygen. FIO2 is typically maintained below 0.5 even with mechanical ventilation, to avoid oxygen toxicity, but there are applications when up to 100% is routinely used.
Blood gas tension refers to the partial pressure of gases in blood. There are several significant purposes for measuring gas tension. The most common gas tensions measured are oxygen tension (PxO2), carbon dioxide tension (PxCO2) and carbon monoxide tension (PxCO). The subscript x in each symbol represents the source of the gas being measured: "a" meaning arterial, "A" being alveolar, "v" being venous, and "c" being capillary. Blood gas tests (such as arterial blood gas tests) measure these partial pressures.