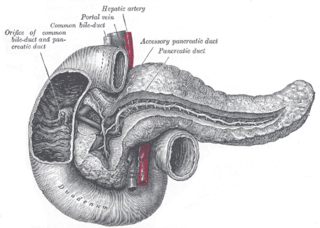
In vertebrates, the gallbladder, also known as the cholecyst, is a small hollow organ where bile is stored and concentrated before it is released into the small intestine. In humans, the pear-shaped gallbladder lies beneath the liver, although the structure and position of the gallbladder can vary significantly among animal species. It receives and stores bile, produced by the liver, via the common hepatic duct, and releases it via the common bile duct into the duodenum, where the bile helps in the digestion of fats.

A bile duct is any of a number of long tube-like structures that carry bile, and is present in most vertebrates.

A gallstone is a stone formed within the gallbladder from precipitated bile components. The term cholelithiasis may refer to the presence of gallstones or to any disease caused by gallstones, and choledocholithiasis refers to the presence of migrated gallstones within bile ducts.

Cholecystectomy is the surgical removal of the gallbladder. Cholecystectomy is a common treatment of symptomatic gallstones and other gallbladder conditions. In 2011, cholecystectomy was the eighth most common operating room procedure performed in hospitals in the United States. Cholecystectomy can be performed either laparoscopically, or via an open surgical technique.

Endoscopic retrograde cholangiopancreatography (ERCP) is a technique that combines the use of endoscopy and fluoroscopy to diagnose and treat certain problems of the biliary or pancreatic ductal systems. It is primarily performed by highly skilled and specialty trained gastroenterologists. Through the endoscope, the physician can see the inside of the stomach and duodenum, and inject a contrast medium into the ducts in the biliary tree and pancreas so they can be seen on radiographs.

The bile duct is a part of the biliary tract. It is formed by the union of the common hepatic duct and cystic duct. It ends by uniting with the pancreatic duct to form the hepatopancreatic ampulla. It possesses its own sphincter to enable regulation of bile flow.
Courvoisier's principle states that a painless palpably enlarged gallbladder accompanied with mild jaundice is unlikely to be caused by gallstones. Usually, the term is used to describe the physical examination finding of the right-upper quadrant of the abdomen. This sign implicates possible malignancy of the gallbladder or pancreas and the swelling is unlikely due to gallstones.

A pancreaticoduodenectomy, also known as a Whipple procedure, is a major surgical operation most often performed to remove cancerous tumours from the head of the pancreas. It is also used for the treatment of pancreatic or duodenal trauma, or chronic pancreatitis. Due to the shared blood supply of organs in the proximal gastrointestinal system, surgical removal of the head of the pancreas also necessitates removal of the duodenum, proximal jejunum, gallbladder, and, occasionally, part of the stomach.

Common bile duct stone, also known as choledocholithiasis, is the presence of gallstones in the common bile duct (CBD). This condition can cause jaundice and liver cell damage. Treatments include choledocholithotomy and endoscopic retrograde cholangiopancreatography (ERCP).
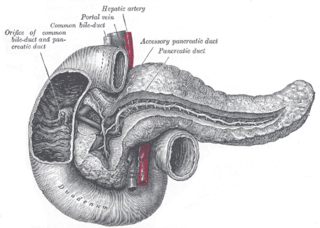
The pancreatic duct, or duct of Wirsung, is a duct joining the pancreas to the common bile duct. This supplies it with pancreatic juice from the exocrine pancreas, which aids in digestion.

A biliary fistula is a type of fistula in which bile flows along an abnormal connection from the bile ducts into nearby hollow structure. Types of biliary fistula include:

Ascending cholangitis, also known as acute cholangitis or simply cholangitis, is inflammation of the bile duct, usually caused by bacteria ascending from its junction with the duodenum. It tends to occur if the bile duct is already partially obstructed by gallstones.

The biliary tract refers to the liver, gallbladder and bile ducts, and how they work together to make, store and secrete bile. Bile consists of water, electrolytes, bile acids, cholesterol, phospholipids and conjugated bilirubin. Some components are synthesized by hepatocytes ; the rest are extracted from the blood by the liver.

Percutaneous transhepatic cholangiography, percutaneous hepatic cholangiogram (PTHC) is a radiological technique used to visualize the anatomy of the biliary tract. A contrast medium is injected into a bile duct in the liver, after which X-rays are taken. It allows access to the biliary tree in cases where endoscopic retrograde cholangiopancreatography has been unsuccessful. Initially reported in 1937, the procedure became popular in 1952.
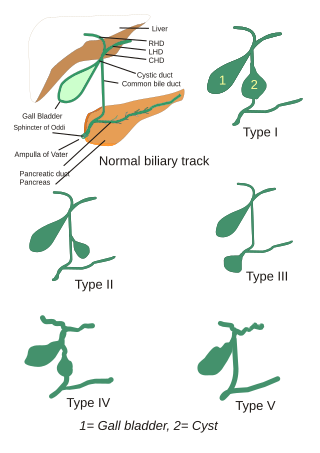
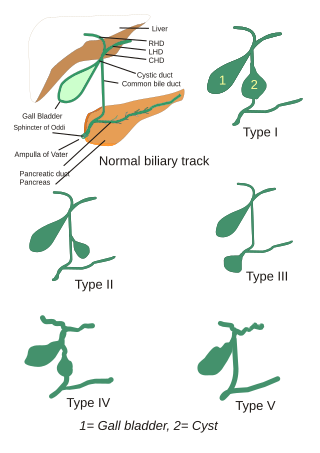
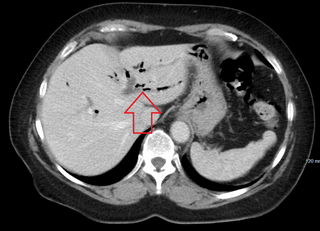
Choledochal cysts are congenital conditions involving cystic dilatation of bile ducts. They are uncommon in western countries but not as rare in East Asian nations like Japan and China.

Periampullary cancer is a cancer that forms near the ampulla of Vater, an enlargement of the ducts from the liver and pancreas where they join and enter the small intestine. It consists of:
- ampullary tumour from ampulla of Vater
- cancer of lower common bile duct
- duodenal cancer adjacent to ampulla
- carcinoma head of pancreas
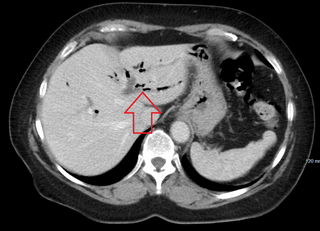
Pneumobilia is the presence of gas in the biliary system. It is typically detected by ultrasound or a radiographic imaging exam, such as CT, or MRI. It is a common finding in patients that have recently undergone biliary surgery or endoscopic biliary procedure. While the presence of air within biliary system is not harmful, this finding may alternatively suggest a pathological process, such as a biliary-enteric anastomosis, an infection of the biliary system, an incompetent sphincter of Oddi, or spontaneous biliary-enteric fistula.

Sphincter of Oddi dysfunction refers to a group of functional disorders leading to abdominal pain due to dysfunction of the Sphincter of Oddi: functional biliary sphincter of Oddi and functional pancreatic sphincter of Oddi disorder. The sphincter of Oddi is a sphincter muscle, a circular band of muscle at the bottom of the biliary tree which controls the flow of pancreatic juices and bile into the second part of the duodenum. The pathogenesis of this condition is recognized to encompass stenosis or dyskinesia of the sphincter of Oddi ; consequently the terms biliary dyskinesia, papillary stenosis, and postcholecystectomy syndrome have all been used to describe this condition. Both stenosis and dyskinesia can obstruct flow through the sphincter of Oddi and can therefore cause retention of bile in the biliary tree and pancreatic juice in the pancreatic duct.

Biliary endoscopic sphincterotomy is a procedure where the sphincter of Oddi and the segment of the common bile duct where it enters the duodenum are cannulated and then cut with a sphincterotome, a device that includes a wire which cuts with an electric current (electrocautery).

Antrectomy, also called distal gastrectomy, is a type of gastric resection surgery that involves the removal of the stomach antrum to treat gastric diseases causing the damage, bleeding, or blockage of the stomach. This is performed using either the Billroth I (BI) or Billroth II (BII) reconstruction method. Quite often, antrectomy is used alongside vagotomy to maximise its safety and effectiveness. Modern antrectomies typically have a high success rate and low mortality rate, but the exact numbers depend on the specific conditions being treated.