Related Research Articles
Cranial nerves are the nerves that emerge directly from the brain, of which there are conventionally considered twelve pairs. Cranial nerves relay information between the brain and parts of the body, primarily to and from regions of the head and neck, including the special senses of vision, taste, smell, and hearing.

Bell's palsy is a type of facial paralysis that results in a temporary inability to control the facial muscles on the affected side of the face. Symptoms can vary from mild to severe. They may include muscle twitching, weakness, or total loss of the ability to move one or, in rare cases, both sides of the face. Other symptoms include drooping of the eyelid, a change in taste, and pain around the ear. Typically symptoms come on over 48 hours. Bell's palsy can trigger an increased sensitivity to sound known as hyperacusis.
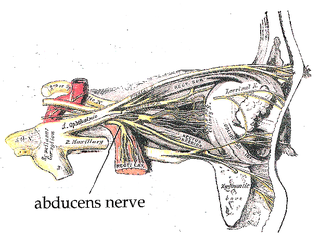
The abducens nerve is the sixth cranial nerve (CNVI), in humans, that controls the movement of the lateral rectus muscle, one of the extraocular muscles responsible for outward gaze. It is a somatic efferent nerve.

The facial nerve is the seventh cranial nerve, or simply CN VII. It emerges from the pons of the brainstem, controls the muscles of facial expression, and functions in the conveyance of taste sensations from the anterior two-thirds of the tongue. The nerves typically travels from the pons through the facial canal in the temporal bone and exits the skull at the stylomastoid foramen. It arises from the brainstem from an area posterior to the cranial nerve VI and anterior to cranial nerve VIII.

Peroneal nerve paralysis is a paralysis on common fibular nerve that affects patient’s ability to lift the foot at the ankle. The condition was named after Friedrich Albert von Zenker. Peroneal nerve paralysis usually leads to neuromuscular disorder, peroneal nerve injury, or foot drop which can be symptoms of more serious disorders such as nerve compression. The origin of peroneal nerve palsy has been reported to be associated with musculoskeletal injury or isolated nerve traction and compression. Also it has been reported to be mass lesions and metabolic syndromes. Peroneal nerve is most commonly interrupted at the knee and possibly at the joint of hip and ankle. Most studies reported that about 30% of peroneal nerve palsy is followed from knee dislocations.
Electroneuronography or electroneurography (ENoG) is a neurological non-invasive test used to study the facial nerve in cases of muscle weakness in one side of the face. The technique of electroneuronography was first used by Esslen and Fisch in 1979 to describe a technique that examines the integrity and conductivity of peripheral nerves. In modern use, ENoG is used to describe study of the facial nerve, while the term nerve conduction study is employed for other nerves.

Facial nerve paralysis is a common problem that involves the paralysis of any structures innervated by the facial nerve. The pathway of the facial nerve is long and relatively convoluted, so there are a number of causes that may result in facial nerve paralysis. The most common is Bell's palsy, a disease of unknown cause that may only be diagnosed by exclusion of identifiable serious causes.
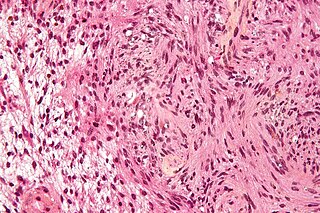
Neurotmesis is part of Seddon's classification scheme used to classify nerve damage. It is the most serious nerve injury in the scheme. In this type of injury, both the nerve and the nerve sheath are disrupted. While partial recovery may occur, complete recovery is impossible.
Axonotmesis is an injury to the peripheral nerve of one of the extremities of the body. The axons and their myelin sheath are damaged in this kind of injury, but the endoneurium, perineurium and epineurium remain intact. Motor and sensory functions distal to the point of injury are completely lost over time leading to Wallerian degeneration due to ischemia, or loss of blood supply. Axonotmesis is usually the result of a more severe crush or contusion than neurapraxia.
Hemifacial spasm (HFS) is a rare neuromuscular disease characterized by irregular, involuntary muscle contractions (spasms) on one side (hemi-) of the face (-facial). The facial muscles are controlled by the facial nerve, which originates at the brainstem and exits the skull below the ear where it separates into five main branches.
Microvascular decompression (MVD), also known as the Jannetta procedure, is a neurosurgical procedure used to treat trigeminal neuralgia a pain syndrome characterized by severe episodes of intense facial pain, and hemifacial spasm. The procedure is also used experimentally to treat tinnitus and vertigo caused by vascular compression on the vestibulocochlear nerve.
Neurofibromatosis type II is a genetic condition that may be inherited or may arise spontaneously, and causes benign tumors of the brain, spinal cord, and peripheral nerves. The types of tumors frequently associated with NF2 include vestibular schwannomas, meningiomas, and ependymomas. The main manifestation of the condition is the development of bilateral benign brain tumors in the nerve sheath of the cranial nerve VIII, which is the "auditory-vestibular nerve" that transmits sensory information from the inner ear to the brain. Besides, other benign brain and spinal tumors occur. Symptoms depend on the presence, localisation and growth of the tumor(s), in which multiple cranial nerves can be involved. Many people with this condition also experience vision problems. Neurofibromatosis type II is caused by mutations of the "Merlin" gene, which seems to influence the form and movement of cells. The principal treatments consist of neurosurgical removal of the tumors and surgical treatment of the eye lesions. Historically the underlying disorder has not had any therapy due to the cell function caused by the genetic mutation.

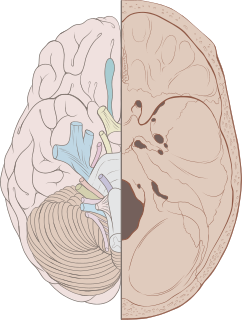
Brain herniation is a potentially deadly side effect of very high pressure within the skull that occurs when a part of the brain is squeezed across structures within the skull. The brain can shift across such structures as the falx cerebri, the tentorium cerebelli, and even through the foramen magnum. Herniation can be caused by a number of factors that cause a mass effect and increase intracranial pressure (ICP): these include traumatic brain injury, intracranial hemorrhage, or brain tumor.

A brachial plexus injury (BPI), also known as brachial plexus lesion, is an injury to the brachial plexus, the network of nerves that conducts signals from the spinal cord to the shoulder, arm and hand. These nerves originate in the fifth, sixth, seventh and eighth cervical (C5–C8), and first thoracic (T1) spinal nerves, and innervate the muscles and skin of the chest, shoulder, arm and hand.

Sixth nerve palsy, or abducens nerve palsy, is a disorder associated with dysfunction of cranial nerve VI, which is responsible for causing contraction of the lateral rectus muscle to abduct the eye. The inability of an eye to turn outward, results in a convergent strabismus or esotropia of which the primary symptom is diplopia in which the two images appear side-by-side. Thus, the diplopia is horizontal and worse in the distance. Diplopia is also increased on looking to the affected side and is partly caused by overaction of the medial rectus on the unaffected side as it tries to provide the extra innervation to the affected lateral rectus. These two muscles are synergists or "yoke muscles" as both attempt to move the eye over to the left or right. The condition is commonly unilateral but can also occur bilaterally.

Ptosis, also known as blepharoptosis, is a drooping or falling of the upper eyelid. The drooping may be worse after being awake longer when the individual's muscles are tired. This condition is sometimes called "lazy eye", but that term normally refers to the condition amblyopia. If severe enough and left untreated, the drooping eyelid can cause other conditions, such as amblyopia or astigmatism. This is why it is especially important for this disorder to be treated in children at a young age, before it can interfere with vision development.

Ulnar nerve entrapment is a condition where the ulnar nerve becomes physically trapped or pinched, resulting in pain, numbness, or weakness, primarily affecting the little finger and ring finger of the hand. Entrapment may occur at any point from the spine at cervical vertebra C7 to the wrist; the most common point of entrapment is in the elbow. Prevention is mostly through correct posture and avoiding repetitive or constant strain. Treatment is usually conservative, including medication, activity modification and exercise, but may sometimes include surgery. Prognosis is generally good, with mild to moderate symptoms often resolving spontaneously.
Synkinesis is a neurological symptom in which a voluntary muscle movement causes the simultaneous involuntary contraction of other muscles. An example might be smiling inducing an involuntary contraction of the eye muscles, causing a person to squint when smiling. Facial and extraocular muscles are affected most often; in rare cases, a person's hands might perform mirror movements.
The cerebellopontine angle syndrome is a distinct neurological syndrome of deficits that can arise due to the closeness of the cerebellopontine angle to specific cranial nerves. Indications include unilateral hearing loss (85%), speech impediments, disequilibrium, tremors or other loss of motor control. The cerebellopontine angle cistern is a subarachnoid cistern formed by the cerebellopontine angle that lies between the cerebellum and the pons. It is filled with cerebrospinal fluid and is a common site for the growth of acoustic neuromas or schwannomas.

Cranial nerve disease is an impaired functioning of one of the twelve cranial nerves. Although it could theoretically be considered a mononeuropathy, it is not considered as such under MeSH.
References
- ↑ Gopen Q (15 December 2013). Fundamental Otology: Pediatric and Adult Practice. Jaypee Brothers Medical Publishers Pvt. Ltd. p. 413. ISBN 978-93-5152-046-7.
- 1 2 3 Grewal DS (14 May 2014). Atlas of Surgery of the Facial Nerve: An Otolaryngologist's Perspective. Jaypee Brothers Publishers. p. 35. ISBN 978-93-5090-580-7.
- ↑ Ballenger's Otorhinolaryngology (17 ed.). BC Decker Inc. pp. 404–405. ISBN 9781550093377.
- ↑ May, M (1979). "Total facial nerve exploration: Transmastoid, Extralabyrinthine and sub temporal indication and results". The Laryngoscope. 89 (6 Pt 1): 906–917. doi:10.1288/00005537-197906000-00006. PMID 312987. S2CID 6590439.
- Scott-Brown's Otorhinolaryngology: Head and Neck Surgery (3 volume set) (7th ed.). Hodder Arnold. 2008. pp. 4022 to 4024. ISBN 9780340808931.
- Glasscock-Shambaugh Surgery of the Ear. W.B.Shaunbers Company. 1967. ISBN 0721681417.
- Disease of ENT and Head and Neak Surgery (6th ed.). Elsevier. October 2013. p. 99. ISBN 9788131234310.
- McNeill, Roger (May 1974). "Facial Nerve Decompression". The Journal of Laryngology & Otology. 88 (5): 445–455. doi:10.1017/S0022215100078919. PMID 4830849.
- Paul, P; Sabrigirish, K; Choudhury, B; Upadhyay, K; Raina, S (2010). "Facial Nerve Decompression via Posterior Tympanotomy Approach". The Indian Journal of Neurotrauma. 7. doi:10.1016/S0973-0508(10)80019-X.