Related Research Articles

Wernicke-Korsakoff syndrome (WKS) is the combined presence of Wernicke encephalopathy (WE) and alcoholic Korsakoff syndrome. Due to the close relationship between these two disorders, people with either are usually diagnosed with WKS as a single syndrome. It mainly causes vision changes, ataxia and impaired memory.

Korsakoff syndrome (KS) is a disorder of the central nervous system characterized by amnesia, deficits in explicit memory, and confabulation. This neurological disorder is caused by a deficiency of thiamine (vitamin B1) in the brain, and it is typically associated with and exacerbated by the prolonged, excessive ingestion of alcohol. Korsakoff syndrome is often accompanied by Wernicke encephalopathy; this combination is called Wernicke–Korsakoff syndrome.
Wernicke encephalopathy (WE), also Wernicke's encephalopathy, or wet brain is the presence of neurological symptoms caused by biochemical lesions of the central nervous system after exhaustion of B-vitamin reserves, in particular thiamine (vitamin B1). The condition is part of a larger group of thiamine deficiency disorders that includes beriberi, in all its forms, and alcoholic Korsakoff syndrome. When it occurs simultaneously with alcoholic Korsakoff syndrome it is known as Wernicke–Korsakoff syndrome.

Leigh syndrome is an inherited neurometabolic disorder that affects the central nervous system. It is named after Archibald Denis Leigh, a British neuropsychiatrist who first described the condition in 1951. Normal levels of thiamine, thiamine monophosphate, and thiamine diphosphate are commonly found, but there is a reduced or absent level of thiamine triphosphate. This is thought to be caused by a blockage in the enzyme thiamine-diphosphate kinase, and therefore treatment in some patients would be to take thiamine triphosphate daily. While the majority of patients typically exhibit symptoms between the ages of 3 and 12 months, instances of adult onset have also been documented.

Neuroprotection refers to the relative preservation of neuronal structure and/or function. In the case of an ongoing insult the relative preservation of neuronal integrity implies a reduction in the rate of neuronal loss over time, which can be expressed as a differential equation.

A neurodegenerative disease is caused by the progressive loss of neurons, in the process known as neurodegeneration. Neuronal damage may also ultimately result in their death. Neurodegenerative diseases include amyotrophic lateral sclerosis, multiple sclerosis, Parkinson's disease, Alzheimer's disease, Huntington's disease, multiple system atrophy, tauopathies, and prion diseases. Neurodegeneration can be found in the brain at many different levels of neuronal circuitry, ranging from molecular to systemic. Because there is no known way to reverse the progressive degeneration of neurons, these diseases are considered to be incurable; however research has shown that the two major contributing factors to neurodegeneration are oxidative stress and inflammation. Biomedical research has revealed many similarities between these diseases at the subcellular level, including atypical protein assemblies and induced cell death. These similarities suggest that therapeutic advances against one neurodegenerative disease might ameliorate other diseases as well.
The biochemistry of Alzheimer's disease, the most common cause of dementia, is not yet very well understood. Alzheimer's disease (AD) has been identified as a proteopathy: a protein misfolding disease due to the accumulation of abnormally folded amyloid beta (Aβ) protein in the brain. Amyloid beta is a short peptide that is an abnormal proteolytic byproduct of the transmembrane protein amyloid-beta precursor protein (APP), whose function is unclear but thought to be involved in neuronal development. The presenilins are components of proteolytic complex involved in APP processing and degradation.

Benfotiamine is a synthetic, fat-soluble, S-acyl derivative of thiamine that is approved in some countries as a medication or dietary supplement to treat diabetic sensorimotor polyneuropathy. Benfotiamine was developed in late 1950s in Japan.

Brain mitochondrial carrier protein 1 is a protein that in humans is encoded by the SLC25A14 gene.
Nervous system diseases, also known as nervous system or neurological disorders, refers to a small class of medical conditions affecting the nervous system. This category encompasses over 600 different conditions, including genetic disorders, infections, cancer, seizure disorders, conditions with a cardiovascular origin, congenital and developmental disorders, and degenerative disorders.
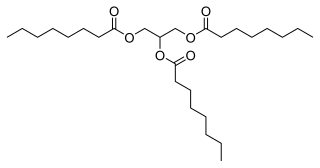
Axona was previously marketed as a medical food for the clinical dietary management of the impairment of metabolic processes associated with mild to moderate Alzheimer's disease. It is a proprietary formulation of fractionated palm kernel oil, a medium-chain triglyceride. Cericin, the company that makes Axona, states that during digestion, caprylic triglyceride is broken down into ketones, which provide an alternative energy source for the brain. Its use is based on the idea that the brain's ability to use its normal energy source, glucose, is impaired in Alzheimer's disease. Axona was first sold in March 2009.
Samuel E. Gandy, is a neurologist, cell biologist, Alzheimer's disease (AD) researcher and expert in the metabolism of the sticky substance called amyloid that clogs the brain in patients with Alzheimer's. His team discovered the first drugs that could lower the formation of amyloid.

Anne Buckingham Young is an American physician and neuroscientist who has made major contributions to the study of neurodegenerative diseases, with a focus on movement disorders like Huntington's disease and Parkinson's disease. Young completed her undergraduate studies at Vassar College and earned a dual MD/PhD from Johns Hopkins Medical School. She has held faculty positions at University of Michigan and Harvard University. She became the first female chief of service at Massachusetts General Hospital when she was appointed Chief of Neurology in 1991. She retired from this role and from clinical service in 2012. She is a member of many academic societies and has won numerous awards. Young is also the only person to have been president of both the international Society for Neuroscience and the American Neurological Association.

Nutritional neuroscience is the scientific discipline that studies the effects various components of the diet such as minerals, vitamins, protein, carbohydrates, fats, dietary supplements, synthetic hormones, and food additives have on neurochemistry, neurobiology, behavior, and cognition.
John P. Blass, physician, biochemist and neurochemist, was born on February 21, 1937, in Vienna, Austria, and deceased March 12, 2023, in New York City. Both his parents were physicians; his father, Gustaf Blass, was a prominent Viennese radiologist and his mother, Jolan Wirth Blass, a student of Sigmund Freud, was a psychoanalyst originally from Budapest. The family then moved to Stamford, Connecticut. Both parents practiced psychiatry, Gustaf in a private sanitarium in Stamford and Jolan as a child psychiatrist in New York City and Connecticut. He is survived by his wife, son and two granddaughters.
Relatively speaking, the brain consumes an immense amount of energy in comparison to the rest of the body. The mechanisms involved in the transfer of energy from foods to neurons are likely to be fundamental to the control of brain function. Human bodily processes, including the brain, all require both macronutrients, as well as micronutrients.
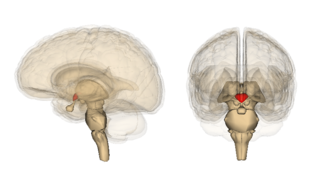
Alcohol-related brain damage alters both the structure and function of the brain as a result of the direct neurotoxic effects of alcohol intoxication or acute alcohol withdrawal. Increased alcohol intake is associated with damage to brain regions including the frontal lobe, limbic system, and cerebellum, with widespread cerebral atrophy, or brain shrinkage caused by neuron degeneration. This damage can be seen on neuroimaging scans.

Rajiv Ratan is an Indian American academic, professor, administrator and scientist based in New York. He is the Burke Professor of Neurology and Neuroscience at Weill Cornell Medicine. Since 2003, he has served as the executive director of Burke Neurological Institute and as a member of the Council of Affiliated Deans of Weill Cornell Medicine.
Lary Walker is an American neuroscientist and researcher at Emory University in Atlanta, Georgia. He is Associate Director of the Goizueta Alzheimer's Disease Research Center at Emory, and he is known for his research on the role of abnormal proteins in the causation of Alzheimer's disease.
Ana Cristina Rego is a Portuguese neurologist. She is a professor at the University of Coimbra in Portugal and is head of the research group on Mitochondria and Neurodegenerative disorders, researching on topics such as Alzheimer's disease, Huntingdon's disease, and Parkinson's disease. She is presently president of the Portuguese Society of Neuroscience.
References
- 1 2 3 4 "Gary E. Gibson". Burke Neurological Institute.
- 1 2 3 4 "Gibson, Gary E." Weill Cornell Medicine .
- ↑ "Alzheimer's is a crisis in NY. Congress must continue to help". AOL . 11 October 2024.
- ↑ "Novel Treatment Approach to Alzheimer's Disease Uses Vitamin B1 Derivative". University of California, San Diego .
- ↑ George, Judy. "Dietary Thiamine Linked With Cognition". MedPage Today .
- ↑ Gibson, G. E.; Hirsch, J. A.; Fonzetti, P.; Jordon, B. D.; Cirio, R. T.; Elder, J. (2016). "Vitamin B1 (thiamine) and dementia". Annals of the New York Academy of Sciences. 1367 (1): 21–30. Bibcode:2016NYASA1367...21G. doi:10.1111/nyas.13031. PMC 4846521 . PMID 26971083.
- ↑ "Alzheimers disease study tests drug made in White Plains NY lab". The Journal News .
- ↑ Hall, Phil (28 July 2022). "Burke Neurological Institute receives grant to pursue benfotiamine research". Westfair Communications.
- ↑ "Golf Outing Raises $7,000 For Alzheimer's Research At Burke Rehab Center". Daily Voice (American hyperlocal news) . 3 January 2015.
- ↑ "Burke Neurological Institute Receives a $45 Million NIH Grant". Business Wire .
- ↑ "Gibson Lab". Burke Neurological Institute.
- ↑ "Important new Alzheimer's study focuses on Westchester scientist's work. Who qualifies?". The Journal News .
- ↑ "Gary E. Gibson". Research.
- ↑ "New Research from Burke Neurological Institute Suggests Raising Vitamin B1 Levels May Provide Novel Treatment for Alzheimer's Disease". BioSpace. 20 August 2021.
- ↑ Inacio, Patricia Inacio (14 July 2022). "$45M Grant Funds Trial of Vitamin B1 Precursor for Cognitive Decline | Alzheimer's Clinical Trial of Benfotiamine Gets $45M NIH Grant | Alzheimer's News Today". alzheimersnewstoday.com.