Related Research Articles

Dementia is the general name for a decline in cognitive abilities that impacts a person's ability to perform everyday activities. This typically involves problems with memory, thinking, and behavior. Aside from memory impairment and a disruption in thought patterns, the most common symptoms include emotional problems, difficulties with language, and decreased motivation. The symptoms may be described as occurring in a continuum over several stages. Dementia ultimately has a significant effect on the individual, caregivers, and on social relationships in general. A diagnosis of dementia requires the observation of a change from a person's usual mental functioning and a greater cognitive decline than what is caused by normal aging.
Delirium is a specific state of acute confusion attributable to the direct physiological consequence of a medical condition, effects of a psychoactive substance, or multiple causes, which usually develops over the course of hours to days. As a syndrome, delirium presents with disturbances in attention, awareness, and higher-order cognition. People with delirium may experience other neuropsychiatric disturbances, including changes in psychomotor activity, disrupted sleep-wake cycle, emotional disturbances, disturbances of consciousness, or, altered state of consciousness, as well as perceptual disturbances, although these features are not required for diagnosis.
The mental status examination (MSE) is an important part of the clinical assessment process in neurological and psychiatric practice. It is a structured way of observing and describing a patient's psychological functioning at a given point in time, under the domains of appearance, attitude, behavior, mood and affect, speech, thought process, thought content, perception, cognition, insight, and judgment. There are some minor variations in the subdivision of the MSE and the sequence and names of MSE domains.
Cognitive disorders (CDs), also known as neurocognitive disorders (NCDs), are a category of mental health disorders that primarily affect cognitive abilities including learning, memory, perception, and problem-solving. Neurocognitive disorders include delirium, mild neurocognitive disorders, and major neurocognitive disorder. They are defined by deficits in cognitive ability that are acquired, typically represent decline, and may have an underlying brain pathology. The DSM-5 defines six key domains of cognitive function: executive function, learning and memory, perceptual-motor function, language, complex attention, and social cognition.
The mini–mental state examination (MMSE) or Folstein test is a 30-point questionnaire that is used extensively in clinical and research settings to measure cognitive impairment. It is commonly used in medicine and allied health to screen for dementia. It is also used to estimate the severity and progression of cognitive impairment and to follow the course of cognitive changes in an individual over time; thus making it an effective way to document an individual's response to treatment. The MMSE's purpose has been not, on its own, to provide a diagnosis for any particular nosological entity.
The Abbreviated Mental Test score (AMTS) is a 10-point test for rapidly assessing elderly patients for the possibility of dementia. It was first used in 1972, and is now sometimes also used to assess for mental confusion and other cognitive impairments.
The Clinical Dementia Rating or CDR is a numeric scale used to quantify the severity of symptoms of dementia.
Cognitive impairment is an inclusive term to describe any characteristic that acts as a barrier to the cognition process or different areas of cognition. Cognition, also known as cognitive function, refers to the mental processes of how a person gains knowledge, uses existing knowledge, and understands things that are happening around them using their thoughts and senses. A cognitive impairment can be in different domains or aspects of a person's cognitive function including memory, attention span, planning, reasoning, decision-making, language, executive functioning, and visuospatial functioning. The term cognitive impairment covers many different diseases and conditions and may also be symptom or manifestation of a different underlying condition. Examples include impairments in overall intelligence ,specific and restricted impairments in cognitive abilities, neuropsychological impairments, or it may describe drug-induced impairment in cognition and memory. Cognitive impairments may be short-term, progressive or permanent.
Schedules for Clinical Assessment in Neuropsychiatry (SCAN) is a set of tools created by WHO aimed at diagnosing and measuring mental illness that may occur in adult life. It is not constructed explicitly for use with either ICD-10 or DSM-IV but can be used for both systems. The SCAN system was originally called PSE, or Present State Examination, but since version 10 (PSE-10), the commonly accepted name has been SCAN. The current version of SCAN is 2.1.
Pseudodementia is a condition where mental cognition can be temporarily decreased. The term pseudodementia is applied to the range of functional psychiatric conditions such as depression, schizophrenia and hysteria that may mimic organic dementia, but are essentially reversible on treatment. Pseudodementia typically involves three cognitive components: memory issues, deficits in executive functioning, and deficits in speech and language. Specific cognitive symptoms might include trouble recalling words or remembering things in general, decreased attentional control and concentration, difficulty completing tasks or making decisions, decreased speed and fluency of speech, and impaired processing speed. People with pseudodementia are typically very distressed about the cognitive impairment they experience. With in this condition, there are two specific treatments that have been found to be effective for the treatment of depression, and these treatments may also be beneficial in the treatment of pseudodementia. Cognitive behavioral therapy (CBT) involves exploring and changing thought patterns and behaviors in order to improve one's mood. Interpersonal therapy focuses on the exploration of an individual's relationships and identifying any ways in which they may be contributing to feelings of depression.
The Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) is a questionnaire that can be filled out by a relative or other supporter of an older person to determine whether that person has declined in cognitive functioning. The IQCODE is used as a screening test for dementia. If the person is found to have significant cognitive decline, then this needs to be followed up with a medical examination to determine whether dementia is present.
Psychological therapies for dementia are starting to gain some momentum. Improved clinical assessment in early stages of Alzheimer's disease and other forms of dementia, increased cognitive stimulation of the elderly, and the prescription of drugs to slow cognitive decline have resulted in increased detection in the early stages. Although the opinions of the medical community are still apprehensive to support cognitive therapies in dementia patients, recent international studies have started to create optimism.
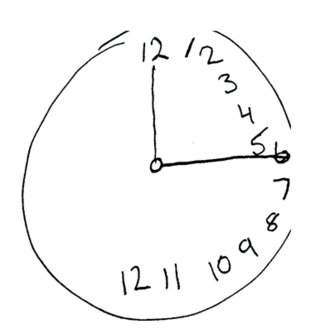
The Montreal Cognitive Assessment (MoCA) is a widely used screening assessment for detecting cognitive impairment. It was created in 1996 by Ziad Nasreddine in Montreal, Quebec. It was validated in the setting of mild cognitive impairment (MCI), and has subsequently been adopted in numerous other clinical settings. This test consists of 30 points and takes 10 minutes for the individual to complete. The original English version is performed in seven steps, which may change in some countries dependent on education and culture. The basics of this test include short-term memory, executive function, attention, focus, and more.
Cognistat, formerly known as the Neurobehavioral Cognitive Status Examination (NCSE), is a cognitive screening test that assesses five cognitive ability areas. The test was first presented in two articles that appeared in the Annals of Internal Medicine in 1987 describing its design rationale and comparing it with the mini–mental state examination (MMSE) in a population of neurosurgical patients.
Florbetaben, a fluorine-18 (18F)-labeled stilbene derivative, trade name NeuraCeq, is a diagnostic radiotracer developed for routine clinical application to visualize β-amyloid plaques in the brain. It is indicated for Positron Emission Tomography (PET) imaging of β-amyloid neuritic plaque density in the brains of adult patients with cognitive impairment who are being evaluated for Alzheimer's disease (AD) and other causes of cognitive impairment. β-amyloid is a key neuropathological hallmark of AD, so markers of β-amyloid plaque accumulation in the brain are useful in distinguishing AD from other causes of dementia. The tracer successfully completed a global multicenter phase 0–III development program and obtained approval in Europe, US and South Korea in 2014.
The Addenbrooke's Cognitive Examination (ACE) and its subsequent versions are neuropsychological tests used to identify cognitive impairment in conditions such as dementia.
The Saint Louis University Mental Status (SLUMS) Exam is a brief screening assessment used to detect cognitive impairment. It was developed in 2006 at the Saint Louis University School of Medicine Division of Geriatric Medicine, in affiliation with a Veterans' Affairs medical center. The test was initially developed using a veteran population, but has since been adopted as a screening tool for any individual displaying signs of mild cognitive impairment. The intended population typically consists of individuals 60 years and above that display any signs of cognitive deficit. Unlike other widely-used cognitive screens, such as the Mini-Mental State Examination and Montreal Cognitive Assessment, the SLUMS is free to access and use by all healthcare professionals.
The Cognitive Abilities Screening Instrument (CASI) is a cognitive test screening for dementia, in monitoring the disease progression, and in providing profiles of cognitive impairment by examining abilities on attention, concentration, orientation, short-term memory, long-term memory, language abilities, visual construction, list-generating fluency, abstraction, and judgment with score ranges of 0 to 100, respectively.
The 4 'A's Test (4AT) is a bedside medical scale used to help determine if a person has positive signs for delirium. The 4AT also includes cognitive test items, making it suitable also for use as a rapid test for cognitive impairment.
References
- 1 2 3 4 5 6 7 Brodaty, H., et al., The GPCOG: a new screening test for dementia designed for general practice. Journal of the American Geriatrics Society , 2002. 50(3): p. 530-4.
- ↑ Brodaty, H., N.M. Kemp, and L.-F. Low, Characteristics of the GPCOG, a screening tool for cognitive impairment. International Journal of Geriatric Psychiatry, 2004. 19(9): p. 870-4.
- ↑ Brodaty, H., et al., "What is the best dementia screening instrument for general practitioners to use?" American Journal of Geriatric Psychiatry , 2006. 14(5): p. 391-400.
- ↑ Lorentz, W.J., J.M. Scanlan, and S. Borson, Brief screening tests for dementia.. Canadian Journal of Psychiatry - Revue Canadienne de Psychiatrie, 2002. 47(8): p. 723-33.
- ↑ Milne, A., et al., Screening for dementia in primary care: a review of the use, efficacy and quality of measures. International Psychogeriatrics, 2008. 20(5): p. 911-26.
- ↑ Borson S., Scanlan J., Brush M. et al: The Mini-Cog: A cognitive “vital signs” measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry 2000; 15:1021-1027
- ↑ Buschke H., Kuslansky G, Katz M et al: Screening for dementia with the Memory Impairment Screen. Neurology 1999; 52: 231-238
- 1 2 3 4 Basic D, Khoo A, Conforti D et al: Rowland Universal Dementia Assessment Scale, Mini-Mental State Examination and General Practitioner Assessment of Cognition in a multicultural cohort of community-dwelling older persons with early dementia. Australian Psychologist 2009; 44(1):40-53
- ↑ Storey J, Rowland J, Basic D et al: The Rowland Universal Dementia Assessment Scale (RUDAS): A multicultural cognitive assessment scale. International Psychogeriatrics 2004; 16: 13-31
- ↑ Thomas P, Hazif-Thomas C, Vieban F et al: Intérêt du GPcog pour le reperage d’une population agée a risque élève de demence. Psychol NeuroPsychiatr Vieil, 2006; 4(1):1-9
- ↑ Pirani A, et al: The validation of the Italian version of the GPCOG (GPCOG-IT): A contribution to cross-national implementation of a screening test for dementia in general practice. Int Psychogeriatr (under revision).