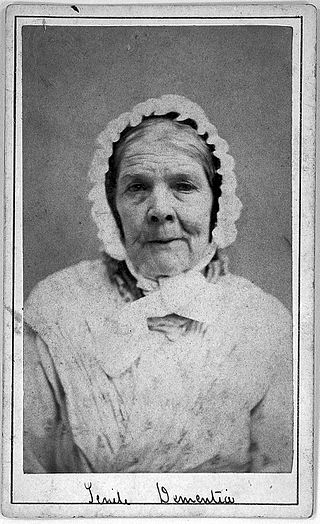
Dementia is a syndrome associated with many neurodegenerative diseases, characterized by a general decline in cognitive abilities that affects a person's ability to perform everyday activities. This typically involves problems with memory, thinking, behavior, and motor control. Aside from memory impairment and a disruption in thought patterns, the most common symptoms of dementia include emotional problems, difficulties with language, and decreased motivation. The symptoms may be described as occurring in a continuum over several stages. Dementia ultimately has a significant effect on the individual, their caregivers, and their social relationships in general. A diagnosis of dementia requires the observation of a change from a person's usual mental functioning and a greater cognitive decline than might be caused by the normal aging process.

Dementia with Lewy bodies (DLB) is a type of dementia characterized by changes in sleep, behavior, cognition, movement, and regulation of automatic bodily functions. Memory loss is not always an early symptom. The disease worsens over time and is usually diagnosed when cognitive impairment interferes with normal daily functioning. Together with Parkinson's disease dementia, DLB is one of the two Lewy body dementias. It is a common form of dementia, but the prevalence is not known accurately and many diagnoses are missed. The disease was first described on autopsy by Kenji Kosaka in 1976, and he named the condition several years later.
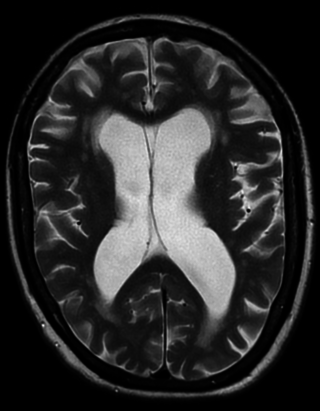
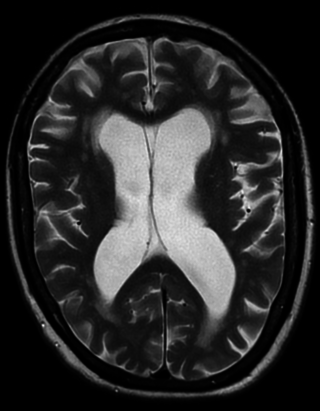
Vascular dementia is dementia caused by a series of strokes. Restricted blood flow due to strokes reduces oxygen and glucose delivery to the brain, causing cell injury and neurological deficits in the affected region. Subtypes of vascular dementia include subcortical vascular dementia, multi-infarct dementia, stroke-related dementia, and mixed dementia.

Donepezil, sold under the brand name Aricept among others, is a medication used to treat dementia of the Alzheimer's type. It appears to result in a small benefit in mental function and ability to function. Use, however, has not been shown to change the progression of the disease. Treatment should be stopped if no benefit is seen. It is taken by mouth or via a transdermal patch.
Cognitive disorders (CDs), also known as neurocognitive disorders (NCDs), are a category of mental health disorders that primarily affect cognitive abilities including learning, memory, perception, and problem-solving. Neurocognitive disorders include delirium, mild neurocognitive disorders, and major neurocognitive disorder. They are defined by deficits in cognitive ability that are acquired, typically represent decline, and may have an underlying brain pathology. The DSM-5 defines six key domains of cognitive function: executive function, learning and memory, perceptual-motor function, language, complex attention, and social cognition.
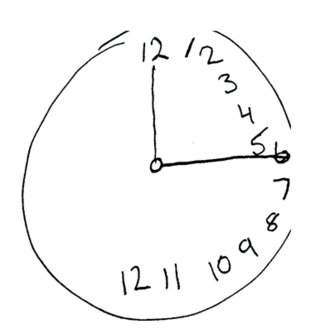
The mini–mental state examination (MMSE) or Folstein test is a 30-point questionnaire that is used extensively in clinical and research settings to measure cognitive impairment. It is commonly used in medicine and allied health to screen for dementia. It is also used to estimate the severity and progression of cognitive impairment and to follow the course of cognitive changes in an individual over time; thus making it an effective way to document an individual's response to treatment. The MMSE's purpose has been not, on its own, to provide a diagnosis for any particular nosological entity.
Age-related memory loss, sometimes described as "normal aging", is qualitatively different from memory loss associated with types of dementia such as Alzheimer's disease, and is believed to have a different brain mechanism.
Mild cognitive impairment (MCI) is a neurocognitive disorder which involves cognitive impairments beyond those expected based on an individual's age and education but which are not significant enough to interfere with instrumental activities of daily living. MCI may occur as a transitional stage between normal aging and dementia, especially Alzheimer's disease. It includes both memory and non-memory impairments. The cause of the disorder remains unclear, as well as both its prevention and treatment, with some 50 percent of people diagnosed with it going on to develop Alzheimer's disease within five years. The diagnosis can also serve as an early indicator for other types of dementia, although MCI may remain stable or even remit.

Alzheimer's disease (AD) is a neurodegenerative disease that usually starts slowly and progressively worsens, and is the cause of 60–70% of cases of dementia. The most common early symptom is difficulty in remembering recent events. As the disease advances, symptoms can include problems with language, disorientation, mood swings, loss of motivation, self-neglect, and behavioral issues. As a person's condition declines, they often withdraw from family and society. Gradually, bodily functions are lost, ultimately leading to death. Although the speed of progression can vary, the average life expectancy following diagnosis is three to twelve years.

The Trail Making Test is a neuropsychological test of visual attention and task switching. It has two parts, in which the subject is instructed to connect a set of 25 dots as quickly as possible while maintaining accuracy. The test can provide information about visual search speed, scanning, speed of processing, mental flexibility, and executive functioning. It is sensitive to cognitive impairment associated with dementia, including Alzheimer's disease.
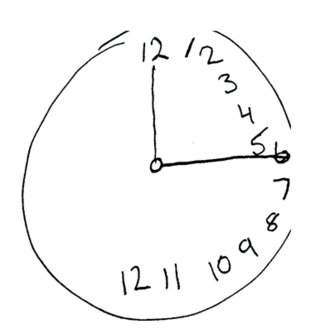
The Montreal Cognitive Assessment (MoCA) is a widely used screening assessment for detecting cognitive impairment. It was created in 1996 by Ziad Nasreddine in Montreal, Quebec. It was validated in the setting of mild cognitive impairment (MCI), and has subsequently been adopted in numerous other clinical settings. This test consists of 30 points and takes 10 minutes for the individual to complete. The original English version is performed in seven steps, which may change in some countries dependent on education and culture. The basics of this test include short-term memory, executive function, attention, focus, and more.
Alzheimer's Disease Neuroimaging Initiative (ADNI) is a multisite study that aims to improve clinical trials for the prevention and treatment of Alzheimer's disease (AD). This cooperative study combines expertise and funding from the private and public sector to study subjects with AD, as well as those who may develop AD and controls with no signs of cognitive impairment. Researchers at 63 sites in the US and Canada track the progression of AD in the human brain with neuroimaging, biochemical, and genetic biological markers. This knowledge helps to find better clinical trials for the prevention and treatment of AD. ADNI has made a global impact, firstly by developing a set of standardized protocols to allow the comparison of results from multiple centers, and secondly by its data-sharing policy which makes available all at the data without embargo to qualified researchers worldwide. To date, over 1000 scientific publications have used ADNI data. A number of other initiatives related to AD and other diseases have been designed and implemented using ADNI as a model. ADNI has been running since 2004 and is currently funded until 2021.
Florbetaben, sold under the brand name Neuraceq, is a diagnostic radiotracer developed for routine clinical application to visualize β-amyloid plaques in the brain. It is a fluorine-18 (18F)-labeled stilbene derivative.
The Addenbrooke's Cognitive Examination (ACE) and its subsequent versions are neuropsychological tests used to identify cognitive impairment in conditions such as dementia.
Visual selective attention is a brain function that controls the processing of retinal input based on whether it is relevant or important. It selects particular representations to enter perceptual awareness and therefore guide behaviour. Through this process, less relevant information is suppressed.
The Saint Louis University Mental Status (SLUMS) Exam is a brief screening assessment used to detect cognitive impairment. It was developed in 2006 at the Saint Louis University School of Medicine Division of Geriatric Medicine, in affiliation with a Veterans' Affairs medical center. The test was initially developed using a veteran population, but has since been adopted as a screening tool for any individual displaying signs of mild cognitive impairment. The intended population typically consists of individuals 60 years and above that display any signs of cognitive deficit. Unlike other widely-used cognitive screens, such as the Mini-Mental State Examination and Montreal Cognitive Assessment, the SLUMS is free to access and use by all healthcare professionals.
The Self-administered Gerocognitive Examination is a brief cognitive assessment instrument for mild cognitive impairment (MCI) and early dementia, created by Douglas Scharre, Professor of Clinical Neurology and Psychiatry at Ohio State University Wexner Medical Center in Columbus, Ohio.
The Alzheimer's Disease Assessment Scale-Cognitive Subscale (ADAS-Cog) is a brief neuropsychological assessment used to assess the severity of cognitive symptoms of dementia. It is one of the most widely used cognitive scales in clinical trials and is considered to be the “gold standard” for assessing antidementia treatments.
The Cogstate Brief Battery (CBB) is a computer-based cognitive assessment used in clinical trials, healthcare, and academic research to measure neurological cognition. It was developed by Cogstate Ltd.
Alzheimer's disease (AD) in African Americans is becoming a rising topic of interest in AD care, support, and scientific research, as African Americans are disproportionately affected by AD. Recent research on AD has shown that there are clear disparities in the disease among racial groups, with higher prevalence and incidence in African Americans than the overall average. Pathologies for Alzheimer’s also seem to manifest differently in African Americans, including with neuroinflammation markers, cognitive decline, and biomarkers. Although there are genetic risk factors for Alzheimer’s, these account for few cases in all racial groups.