Related Research Articles
Hemiparesis, or unilateral paresis, is weakness of one entire side of the body. Hemiplegia is, in its most severe form, complete paralysis of half of the body. Hemiparesis and hemiplegia can be caused by different medical conditions, including congenital causes, trauma, tumors, or stroke.
The Glasgow Coma Scale (GCS) is a clinical scale used to reliably measure a person's level of consciousness after a brain injury.
Activities of daily living (ADLs) is a term used in healthcare to refer to an individual's daily self-care activities. Health professionals often use a person's ability or inability to perform ADLs as a measure of their functional status. The concept of ADLs was originally proposed in the 1950s by Sidney Katz and his team at the Benjamin Rose Hospital in Cleveland, Ohio. Since then, numerous researchers have expanded on the concept of ADLs. For instance, many indexes that assess ADLs now incorporate measures of mobility.

Neurotrauma, brain damage or brain injury (BI) is the destruction or degeneration of brain cells. Brain injuries occur due to a wide range of internal and external factors. In general, brain damage refers to significant, undiscriminating trauma-induced damage.
Rehabilitation of sensory and cognitive function typically involves methods for retraining neural pathways or training new neural pathways to regain or improve neurocognitive functioning that have been diminished by disease or trauma. The main objective outcome for rehabilitation is to assist in regaining physical abilities and improving performance. Three common neuropsychological problems treatable with rehabilitation are attention deficit/hyperactivity disorder (ADHD), concussion, and spinal cord injury. Rehabilitation research and practices are a fertile area for clinical neuropsychologists, rehabilitation psychologists, and others.

Global aphasia is a severe form of nonfluent aphasia, caused by damage to the left side of the brain, that affects receptive and expressive language skills as well as auditory and visual comprehension. Acquired impairments of communicative abilities are present across all language modalities, impacting language production, comprehension, and repetition. Patients with global aphasia may be able to verbalize a few short utterances and use non-word neologisms, but their overall production ability is limited. Their ability to repeat words, utterances, or phrases is also affected. Due to the preservation of the right hemisphere, an individual with global aphasia may still be able to express themselves through facial expressions, gestures, and intonation. This type of aphasia often results from a large lesion of the left perisylvian cortex. The lesion is caused by an occlusion of the left middle cerebral artery and is associated with damage to Broca's area, Wernicke's area, and insular regions which are associated with aspects of language.
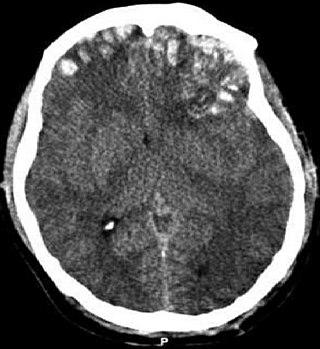
A traumatic brain injury (TBI), also known as an intracranial injury, is an injury to the brain caused by an external force. TBI can be classified based on severity ranging from mild traumatic brain injury (mTBI/concussion) to severe traumatic brain injury. TBI can also be characterized based on mechanism or other features. Head injury is a broader category that may involve damage to other structures such as the scalp and skull. TBI can result in physical, cognitive, social, emotional and behavioral symptoms, and outcomes can range from complete recovery to permanent disability or death.

A minimally conscious state or MCS is a disorder of consciousness distinct from persistent vegetative state and locked-in syndrome. Unlike persistent vegetative state, patients with MCS have partial preservation of conscious awareness. MCS is a relatively new category of disorders of consciousness. The natural history and longer term outcome of MCS have not yet been thoroughly studied. The prevalence of MCS was estimated to be 9 times of PVS cases, or between 112,000 and 280,000 in the US by year 2000.

Muriel Elaine Deutsch Lezak was an American neuropsychologist best known for her book Neuropsychological Assessment, widely accepted as the standard in the field. Her work has centred on the research, assessment, and rehabilitation of brain injury. Lezak was a professor of neurology at the Oregon Health and Science University School of Medicine.
The Kurtzke Expanded Disability Status Scale (EDSS) is a method of quantifying disability in multiple sclerosis. The scale has been developed by John F. Kurtzke. The EDSS is based on a neurological examination by a clinician. However, a number of versions have been developed which enable patient self-administration.

Balance in biomechanics, is an ability to maintain the line of gravity of a body within the base of support with minimal postural sway. Sway is the horizontal movement of the centre of gravity even when a person is standing still. A certain amount of sway is essential and inevitable due to small perturbations within the body or from external triggers. An increase in sway is not necessarily an indicator of dysfunctional balance so much as it is an indicator of decreased sensorimotor control.
Post-traumatic amnesia (PTA) is a state of confusion that occurs immediately following a traumatic brain injury (TBI) in which the injured person is disoriented and unable to remember events that occur after the injury. The person may be unable to state their name, where they are, and what time it is. When continuous memory returns, PTA is considered to have resolved. While PTA lasts, new events cannot be stored in the memory. About a third of patients with mild head injury are reported to have "islands of memory", in which the patient can recall only some events. During PTA, the patient's consciousness is "clouded". Because PTA involves confusion in addition to the memory loss typical of amnesia, the term "post-traumatic confusional state" has been proposed as an alternative.
Dysexecutive syndrome (DES) consists of a group of symptoms, usually resulting from brain damage, that fall into cognitive, behavioural and emotional categories and tend to occur together. The term was introduced by Alan Baddeley to describe a common pattern of dysfunction in executive functions, such as planning, abstract thinking, flexibility and behavioural control. It is thought to be Baddeley's hypothesized working memory system and the central executive that are the hypothetical systems impaired in DES. The syndrome was once known as frontal lobe syndrome; however 'dysexecutive syndrome' is preferred because it emphasizes the functional pattern of deficits over the location of the syndrome in the frontal lobe, which is often not the only area affected.
A psychological injury is the psychological or psychiatric consequence of a traumatic event or physical injury. Such an injury might result from events such as abusive behavior, whistleblower retaliation, bullying, kidnapping, rape, motor vehicular collision or other negligent action. It may cause impairments, disorders, and disabilities perhaps as an exacerbation of a pre-existing condition.
The Wechsler Test of Adult Reading (WTAR) is a neuropsychological assessment tool used to provide a measure of premorbid intelligence, the degree of Intellectual function prior to the onset of illness or disease.
The Westmead Post-traumatic Amnesia Scale (WPTAS) is a brief bedside standardised test that measures length of post-traumatic amnesia (PTA) in people with traumatic brain injury. It consists of twelve questions that assess orientation to person, place and time, and ability to consistently retain new information from one day to another. It is administered once a day, each and every day, until the patient achieves a perfect score across three consecutive days, after which the individual is deemed to have emerged from post-traumatic amnesia. PTA may be deemed to be over on the first day of a recall of 12 for those who have been in PTA for greater than four weeks. The WPTAS is the most common post-traumatic amnesia scale used in Australia and New Zealand.
The Functional Independence Measure (FIM) is an assessment tool that aims to evaluate the functional status of patients throughout the rehabilitation process following a stroke, traumatic brain injury, spinal cord injury or cancer. Its area of use can include skilled nursing facilities and hospitals aimed at acute, sub-acute and rehabilitation care. Performed on admission to and departure from a rehabilitation hospital, it serves as a consistent data collection tool for the comparison of rehabilitation outcomes across the health care continuum. Furthermore, it aims to allow clinicians to track changes in the functional status of patients from the onset of rehab care through discharge and follow-up. The FIM's assessment of degree of disability depends on the patient's score in 18 categories, focusing on motor and cognitive function. Each category or item is rated on a 7-point scale. As such, FIM scores may be interpreted to indicate level of independence or level of burden of care. The scale is used to assess how well a person can carry out basic activities of daily living and thus how dependent he or she will be on help from others. Other areas assessed include the physical like how well patients move and walk, and the cognitive, how well they interact with others, communicate, and process information. FIM was originally made for people who had had strokes, but is used to assess disability in other cases as well.

Outcome measures in rehabilitation medicine are tools used to evaluate the level of disability. They can be beneficial for physicians to judge the path of a patient's recovery, for researchers to compare different management protocols and for politicians in order to find the cost-effectiveness of their decisions.
Rehabilitation psychology is a specialty area of psychology aimed at maximizing the independence, functional status, health, and social participation of individuals with disabilities and chronic health conditions. Assessment and treatment may include the following areas: psychosocial, cognitive, behavioral, and functional status, self-esteem, coping skills, and quality of life. As the conditions experienced by patients vary widely, rehabilitation psychologists offer individualized treatment approaches. The discipline takes a holistic approach, considering individuals within their broader social context and assessing environmental and demographic factors that may facilitate or impede functioning. This approach, integrating both personal and environmental factors, is consistent with the World Health Organization's (WHO) International Classification of Functioning, Disability and Health (ICF).
A pediatric concussion, also known as pediatric mild traumatic brain injury (mTBI), is a head trauma that impacts the brain capacity. Concussion can affect functional, emotional, cognitive and physical factors and can occur in people of all ages. Symptoms following after the concussion vary and may include confusion, disorientation, lightheadedness, nausea, vomiting, blurred vision, loss of consciousness (LOC) and environment sensitivity. Concussion symptoms may vary based on the type, severity and location of the head injury. Concussion symptoms in infants, children, and adolescents often appear immediately after the injury, however, some symptoms may arise multiple days following the injury leading to a concussion. The majority of pediatric patients recover from the symptoms within one month following the injury. 10-30% of children and adolescents have a higher risk of a delayed recovery or of experiencing concussion symptoms that are persisting.
References
- Eliason & Topp (1984) Predictive Validity of Rappaport's Disability Rating Scale in Subjects with Acute Brain Dysfunction. Journal of the American Physical Therapy Association,64:1357-1360
- Nichol, et al. (2011) Measuring Functional and Quality of Life Outcomes Following Major Head Injury: Common Scales and Checklists. Injury, Int J. 42:281-287
- Rappaport, et al. (1982) Disability Rating Scale for Severe Head Trauma Patients: Coma to Community. Archives of Physical Medicine and Rehabilitation, 63:118-123.
- Shulka, Devi, & Agrawal (2011) Outcome Measures for Traumatic Brain Injury. Clinical Neurology and Neurosurgery, 113:435-441
- Wright (2000) The Disability Rating Scale. The Center for Outcome Measurement in Brain Injury. http://www.tbims.org/cmbi/drs%5B%5D.