Squamous-cell skin cancer, also known as cutaneous squamous-cell carcinoma (cSCC), is one of the main types of skin cancer along with basal cell cancer, and melanoma. It usually presents as a hard lump with a scaly top but can also form an ulcer. Onset is often over months. Squamous-cell skin cancer is more likely to spread to distant areas than basal cell cancer. When confined to the outermost layer of the skin, a precancerous or in situ form of cSCC is known as Bowen's disease.

Basal-cell carcinoma (BCC), also known as basal-cell cancer, is the most common type of skin cancer. It often appears as a painless raised area of skin, which may be shiny with small blood vessels running over it. It may also present as a raised area with ulceration. Basal-cell cancer grows slowly and can damage the tissue around it, but it is unlikely to spread to distant areas or result in death.

Head and neck cancer is a group of cancers that starts in the mouth, nose, throat, larynx, sinuses, or salivary glands. Symptoms for head and neck cancer may include a lump or sore that does not heal, a sore throat that does not go away, trouble swallowing, or a change in the voice. There may also be unusual bleeding, facial swelling, or trouble breathing.

Lichen planus (LP) is a chronic inflammatory and immune-mediated disease that affects the skin, nails, hair, and mucous membranes. It is not an actual lichen, and is only named that because it looks like one. It is characterized by polygonal, flat-topped, violaceous papules and plaques with overlying, reticulated, fine white scale, commonly affecting dorsal hands, flexural wrists and forearms, trunk, anterior lower legs and oral mucosa. Although there is a broad clinical range of LP manifestations, the skin and oral cavity remain as the major sites of involvement. The cause is unknown, but it is thought to be the result of an autoimmune process with an unknown initial trigger. There is no cure, but many different medications and procedures have been used in efforts to control the symptoms.

A seborrheic keratosis is a non-cancerous (benign) skin tumour that originates from cells in the outer layer of the skin. Like liver spots, seborrheic keratoses are seen more often as people age.

An epidermoid cyst or epidermal inclusion cyst is a benign cyst usually found on the skin. The cyst develops out of ectodermal tissue. Histologically, it is made of a thin layer of squamous epithelium.

Actinic keratosis (AK), sometimes called solar keratosis or senile keratosis, is a pre-cancerous area of thick, scaly, or crusty skin. Actinic keratosis is a disorder (-osis) of epidermal keratinocytes that is induced by ultraviolet (UV) light exposure (actin-). These growths are more common in fair-skinned people and those who are frequently in the sun. They are believed to form when skin gets damaged by UV radiation from the sun or indoor tanning beds, usually over the course of decades. Given their pre-cancerous nature, if left untreated, they may turn into a type of skin cancer called squamous cell carcinoma. Untreated lesions have up to a 20% risk of progression to squamous cell carcinoma, so treatment by a dermatologist is recommended.
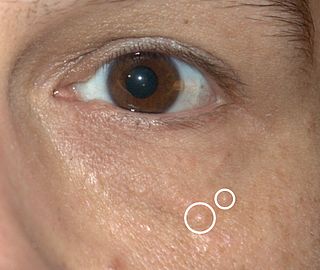
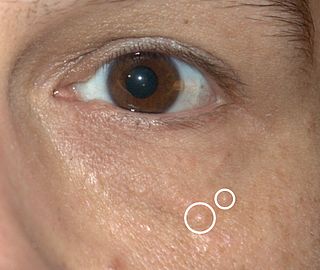
Syringomas are benign eccrine sweat duct tumors, typically found clustered on eyelids, although they may also be found in the armpits, abdomen, chest, neck, scalp or groin area including genitals in a symmetric pattern. They are skin-colored or yellowish firm, rounded bumps, 1–3 mm in diameter, and may be confused with xanthoma, milia, hidrocystoma, trichoepithelioma, and xanthelasma. They are more common in women and are most commonly found in middle-aged Asian women. While they can present at any time in life, they typically present during adolescence. They are usually not associated with any other symptoms although can sometimes cause itchiness or irritation.
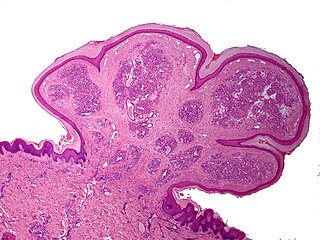
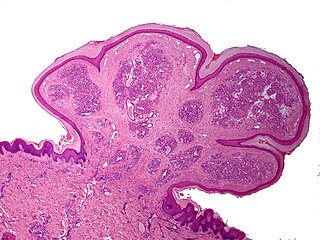
Pyogenic granuloma or pyogenic fibroma is a vascular tumor that occurs on both mucosa and skin, and appears as an overgrowth of tissue due to irritation, physical trauma, or hormonal factors. It is often found to involve the gums, the skin and nasal septum, and has also been found far from the head such as in the thigh.

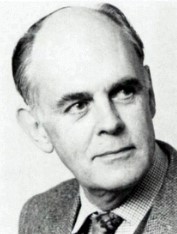
Mohs surgery, developed in 1938 by a general surgeon, Frederic E. Mohs, is microscopically controlled surgery used to treat common types of skin cancer. During the surgery, after each removal of tissue and while the patient waits, the tissue is examined for cancer cells. That examination dictates the decision for additional tissue removal. Mohs surgery is the gold standard method for obtaining complete margin control during removal of a skin cancer using frozen section histology. CCPDMA or Mohs surgery allows for the removal of a skin cancer with very narrow surgical margin and a high cure rate.

Verrucous carcinoma (VC) is an uncommon variant of squamous cell carcinoma. This form of cancer is often seen in those who chew tobacco or use snuff orally, so much so that it is sometimes referred to as "Snuff dipper's cancer".

Vulvar cancer is a cancer of the vulva, the outer portion of the female genitals. It most commonly affects the outer vaginal lips. Less often, the inner vaginal lips, clitoris, or vaginal glands. Symptoms include a lump, itchiness, changes in the skin, or bleeding from the vulva.

Skin biopsy is a biopsy technique in which a skin lesion is removed to be sent to a pathologist to render a microscopic diagnosis. It is usually done under local anesthetic in a physician's office, and results are often available in 4 to 10 days. It is commonly performed by dermatologists. Skin biopsies are also done by family physicians, internists, surgeons, and other specialties. However, performed incorrectly, and without appropriate clinical information, a pathologist's interpretation of a skin biopsy can be severely limited, and therefore doctors and patients may forgo traditional biopsy techniques and instead choose Mohs surgery. There are four main types of skin biopsies: shave biopsy, punch biopsy, excisional biopsy, and incisional biopsy. The choice of the different skin biopsies is dependent on the suspected diagnosis of the skin lesion. Like most biopsies, patient consent and anesthesia are prerequisites.

Discoid lupus erythematosus is the most common type of chronic cutaneous lupus (CCLE), an autoimmune skin condition on the lupus erythematosus spectrum of illnesses. It presents with red, inflamed, coin-shaped patches of skin with a scaling and crusty appearance, most often on the scalp, cheeks, and ears. Hair loss may occur if the lesions are on the scalp. The lesions can then develop severe scarring, and the centre areas may appear lighter in color with a rim darker than the normal skin. These lesions can last for years without treatment.

Cutaneous horns, also known by the Latin name cornu cutaneum, are unusual keratinous skin tumors with the appearance of horns, or sometimes of wood or coral. Formally, this is a clinical diagnosis for a "conical projection above the surface of the skin." They are usually small and localized but can, in very rare cases, be much larger. Although often benign, they can also be malignant or premalignant.
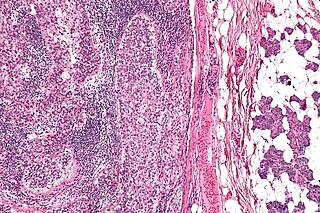
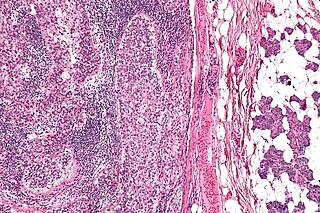
Sebaceous carcinoma, also known as sebaceous gland carcinoma (SGc), sebaceous cell carcinoma, and meibomian gland carcinoma is an uncommon malignant cutaneous tumor. Most are typically about 1.4 cm at presentation. SGc originates from sebaceous glands in the skin and, therefore, may originate anywhere in the body where these glands are found. SGc can be divided into 2 types: periocular and extraocular. The periocular region is rich in sebaceous glands making it a common site of origin. The cause of these lesions in the vast majority of cases is unknown. Occasional cases may be associated with Muir-Torre syndrome. SGc accounts for approximately 0.7% of all skin cancers, and the incidence of SGc is highest in Caucasian, Asian, and Indian populations. Due to the rarity of this tumor and variability in clinical and histological presentation, SGc is often misdiagnosed as an inflammatory condition or a more common neoplasm. SGc is commonly treated with wide local excision or Mohs micrographic surgery, and the relative survival rates at 5 and 10 years are 92.72 and 86.98%, respectively.
Electrodesiccation and curettage is a medical procedure commonly performed by dermatologists, surgeons and general practitioners for the treatment of basal cell cancers and squamous cell cancers of the skin. It provides desiccation, coagulation/cauterization, and curettage to remove lesions from the skin.
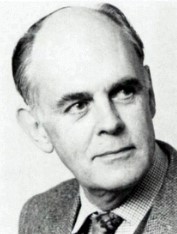
Arthur James Rook FRCP was a leading British dermatologist and the principal author of Rook's Textbook of Dermatology (1968), known as "Rook's", which reached its ninth edition in 2016.