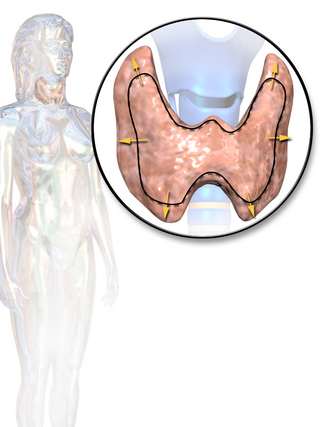
Hyperthyroidism is the condition that occurs due to excessive production of thyroid hormones by the thyroid gland. Thyrotoxicosis is the condition that occurs due to excessive thyroid hormone of any cause and therefore includes hyperthyroidism. Some, however, use the terms interchangeably. Signs and symptoms vary between people and may include irritability, muscle weakness, sleeping problems, a fast heartbeat, heat intolerance, diarrhea, enlargement of the thyroid, hand tremor, and weight loss. Symptoms are typically less severe in the elderly and during pregnancy. An uncommon but life-threatening complication is thyroid storm in which an event such as an infection results in worsening symptoms such as confusion and a high temperature; this often results in death. The opposite is hypothyroidism, when the thyroid gland does not make enough thyroid hormone.

Graves' disease, also known as toxic diffuse goiter, is an autoimmune disease that affects the thyroid. It frequently results in and is the most common cause of hyperthyroidism. It also often results in an enlarged thyroid. Signs and symptoms of hyperthyroidism may include irritability, muscle weakness, sleeping problems, a fast heartbeat, poor tolerance of heat, diarrhea and unintentional weight loss. Other symptoms may include thickening of the skin on the shins, known as pretibial myxedema, and eye bulging, a condition caused by Graves' ophthalmopathy. About 25 to 30% of people with the condition develop eye problems.
Thyroid-stimulating hormone (also known as thyrotropin, thyrotropic hormone, or abbreviated TSH) is a pituitary hormone that stimulates the thyroid gland to produce thyroxine (T4), and then triiodothyronine (T3) which stimulates the metabolism of almost every tissue in the body. It is a glycoprotein hormone produced by thyrotrope cells in the anterior pituitary gland, which regulates the endocrine function of the thyroid.

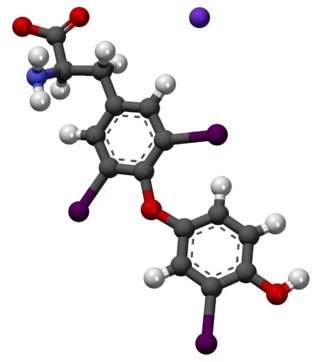
Levothyroxine, also known as L-thyroxine, is a synthetic form of the thyroid hormone thyroxine (T4). It is used to treat thyroid hormone deficiency (hypothyroidism), including a severe form known as myxedema coma. It may also be used to treat and prevent certain types of thyroid tumors. It is not indicated for weight loss. Levothyroxine is taken orally (by mouth) or given by intravenous injection. Levothyroxine has a half-life of 7.5 days when taken daily, so about six weeks is required for it to reach a steady level in the blood.

The Wolff–Chaikoff effect is a presumed reduction in thyroid hormone levels caused by ingestion of a large amount of iodine.

In the United States, a boxed warning is a type of warning that appears near the beginning of the package insert for certain prescription drugs, so called because the U.S. Food and Drug Administration specifies that it is formatted with a 'box' or border around the text to emphasize it is of utmost importance. The FDA can require a pharmaceutical company to place a boxed warning. It is the strongest warning that the FDA requires, and signifies that medical studies indicate that the drug carries a significant risk of preventable, serious or even life-threatening adverse effects.
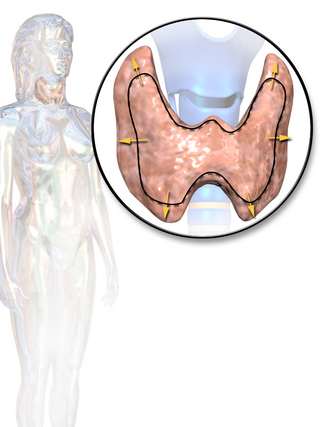
Thyroid disease is a medical condition that affects the function of the thyroid gland. The thyroid gland is located at the front of the neck and produces thyroid hormones that travel through the blood to help regulate many other organs, meaning that it is an endocrine organ. These hormones normally act in the body to regulate energy use, infant development, and childhood development.
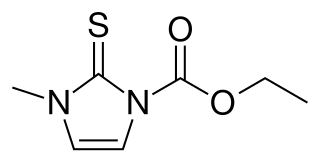
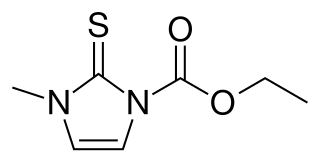
Carbimazole (brand names Neo-Mercazole, Anti-Thyrox, etc.) is used to treat hyperthyroidism. Carbimazole is a pro-drug as after absorption it is converted to the active form, methimazole. Methimazole prevents thyroid peroxidase enzyme from iodinating and coupling the tyrosine residues on thyroglobulin, hence reducing the production of the thyroid hormones T3 and T4 (thyroxine).
Thyroid storm is a rare but severe and life-threatening complication of hyperthyroidism. It occurs when an overactive thyroid leads to hypermetabolism, which can cause death from cardiac arrest or multiple organ failure.
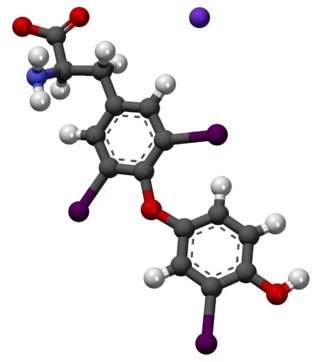
Liothyronine is a manufactured form of the thyroid hormone triiodothyronine (T3). It is most commonly used to treat hypothyroidism and myxedema coma. It can be taken by mouth or by injection into a vein.

De Quervain's thyroiditis, also known as subacute granulomatous thyroiditis or giant cell thyroiditis, is a member of the group of thyroiditis conditions known as resolving thyroiditis. People of all ages and genders may be affected.
Thyroid function tests (TFTs) is a collective term for blood tests used to check the function of the thyroid. TFTs may be requested if a patient is thought to suffer from hyperthyroidism or hypothyroidism, or to monitor the effectiveness of either thyroid-suppression or hormone replacement therapy. It is also requested routinely in conditions linked to thyroid disease, such as atrial fibrillation and anxiety disorder.
Subacute lymphocytic thyroiditis is a form of thyroiditis. Subacute lymphocytic thyroiditis may occur at any age and is more common in females. A variant of subacute lymphocytic thyroiditis occurs postpartum: postpartum thyroiditis. Both of these entities can be considered subtypes of Hashimoto's thyroiditis and have an autoimmune basis. Anti-thyroid antibodies are common in all three and the underlying histology is similar. This disorder should not be confused with de Quervain's thyroiditis which is another form of subacute thyroiditis.
Desiccated thyroid, also known as thyroid extract, is thyroid gland that has been dried and powdered for medical use. It is used to treat hypothyroidism. It is less preferred than levothyroxine. It is taken by mouth. Maximal effects may take up to three weeks to occur.

Subacute thyroiditis refers to a temporal classification of the different forms of thyroiditis based on onset of symptoms. The temporal classification of thyroiditis includes presentation of symptoms in an acute, subacute, or chronic manner. There are also other classification systems for thyroiditis based on factors such as clinical symptoms and underlying etiology.
An antithyroid agent is a hormone inhibitor acting upon thyroid hormones.

Thyroid hormones are any hormones produced and released by the thyroid gland, namely triiodothyronine (T3) and thyroxine (T4). They are tyrosine-based hormones that are primarily responsible for regulation of metabolism. T3 and T4 are partially composed of iodine, derived from food. A deficiency of iodine leads to decreased production of T3 and T4, enlarges the thyroid tissue and will cause the disease known as simple goitre.
Thyroid disease in pregnancy can affect the health of the mother as well as the child before and after delivery. Thyroid disorders are prevalent in women of child-bearing age and for this reason commonly present as a pre-existing disease in pregnancy, or after childbirth. Uncorrected thyroid dysfunction in pregnancy has adverse effects on fetal and maternal well-being. The deleterious effects of thyroid dysfunction can also extend beyond pregnancy and delivery to affect neurointellectual development in the early life of the child. Due to an increase in thyroxine binding globulin, an increase in placental type 3 deioidinase and the placental transfer of maternal thyroxine to the fetus, the demand for thyroid hormones is increased during pregnancy. The necessary increase in thyroid hormone production is facilitated by high human chorionic gonadotropin (hCG) concentrations, which bind the TSH receptor and stimulate the maternal thyroid to increase maternal thyroid hormone concentrations by roughly 50%. If the necessary increase in thyroid function cannot be met, this may cause a previously unnoticed (mild) thyroid disorder to worsen and become evident as gestational thyroid disease. Currently, there is not enough evidence to suggest that screening for thyroid dysfunction is beneficial, especially since treatment thyroid hormone supplementation may come with a risk of overtreatment. After women give birth, about 5% develop postpartum thyroiditis which can occur up to nine months afterwards. This is characterized by a short period of hyperthyroidism followed by a period of hypothyroidism; 20–40% remain permanently hypothyroid.
The signs and symptoms of Graves' disease generally result from the direct and indirect effects of hyperthyroidism; sometimes they are caused by thyroidal conditions, such as Graves' ophthalmopathy, goitre and pretibial myxedema. These clinical manifestations can involve virtually every system in the body. The mechanisms that mediate these effects are not well understood. The severity of the signs and symptoms of hyperthyroidism is related to the duration of the disease, the magnitude of the thyroid hormone excess, and the patient's age. Although the vast majority of patients enjoy significant improvement and remission after proper medical care, health care providers should be aware of variability in the individual response to hyperthyroidism and individual sensitivity to thyroid hormone fluctuations generally. Graves' disease patients can also undergo periods of hypothyroidism, due to the challenges of finding the right dosage of thyroid hormone suppression and/or supplementation. The body's need for thyroid hormone can also change over time, such as in the first months after radioactive iodine treatment (RAI). Thyroid autoimmune diseases can also be volatile: hyperthyroidism can interchange with hypothyroidism and euthyroidism.
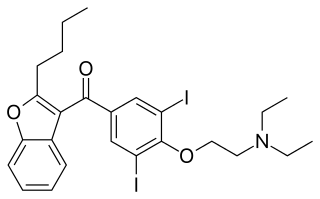
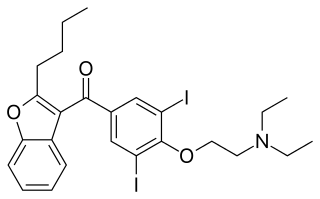
Amiodarone induced thyrotoxicosis (AIT) is a form of hyperthyroidism due to treatment with antiarrhythmic drug, amiodarone.