Related Research Articles

In immunology, an antigen (Ag) is a molecule, moiety, foreign particulate matter, or an allergen, such as pollen, that can bind to a specific antibody or T-cell receptor. The presence of antigens in the body may trigger an immune response.

A DNA vaccine is a type of vaccine that transfects a specific antigen-coding DNA sequence into the cells of an organism as a mechanism to induce an immune response.

A cytotoxic T cell (also known as TC, cytotoxic T lymphocyte, CTL, T-killer cell, cytolytic T cell, CD8+ T-cell or killer T cell) is a T lymphocyte (a type of white blood cell) that kills cancer cells, cells that are infected by intracellular pathogens (such as viruses or bacteria), or cells that are damaged in other ways.

The T helper cells (Th cells), also known as CD4+ cells or CD4-positive cells, are a type of T cell that play an important role in the adaptive immune system. They aid the activity of other immune cells by releasing cytokines. They are considered essential in B cell antibody class switching, breaking cross-tolerance in dendritic cells, in the activation and growth of cytotoxic T cells, and in maximizing bactericidal activity of phagocytes such as macrophages and neutrophils. CD4+ cells are mature Th cells that express the surface protein CD4. Genetic variation in regulatory elements expressed by CD4+ cells determines susceptibility to a broad class of autoimmune diseases.

The major histocompatibility complex (MHC) is a large locus on vertebrate DNA containing a set of closely linked polymorphic genes that code for cell surface proteins essential for the adaptive immune system. These cell surface proteins are called MHC molecules.
An epitope, also known as antigenic determinant, is the part of an antigen that is recognized by the immune system, specifically by antibodies, B cells, or T cells. The part of an antibody that binds to the epitope is called a paratope. Although epitopes are usually non-self proteins, sequences derived from the host that can be recognized are also epitopes.

An antigen-presenting cell (APC) or accessory cell is a cell that displays antigen bound by major histocompatibility complex (MHC) proteins on its surface; this process is known as antigen presentation. T cells may recognize these complexes using their T cell receptors (TCRs). APCs process antigens and present them to T-cells.

MHC class I molecules are one of two primary classes of major histocompatibility complex (MHC) molecules and are found on the cell surface of all nucleated cells in the bodies of vertebrates. They also occur on platelets, but not on red blood cells. Their function is to display peptide fragments of proteins from within the cell to cytotoxic T cells; this will trigger an immediate response from the immune system against a particular non-self antigen displayed with the help of an MHC class I protein. Because MHC class I molecules present peptides derived from cytosolic proteins, the pathway of MHC class I presentation is often called cytosolic or endogenous pathway.
Cross-presentation is the ability of certain professional antigen-presenting cells (mostly dendritic cells) to take up, process and present extracellular antigens with MHC class I molecules to CD8 T cells (cytotoxic T cells). Cross-priming, the result of this process, describes the stimulation of naive cytotoxic CD8+ T cells into activated cytotoxic CD8+ T cells. This process is necessary for immunity against most tumors and against viruses that infect dendritic cells and sabotage their presentation of virus antigens. Cross presentation is also required for the induction of cytotoxic immunity by vaccination with protein antigens, for example, tumour vaccination.
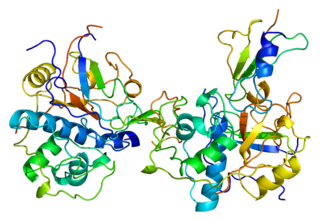
A tetrameric protein is a protein with a quaternary structure of four subunits (tetrameric). Homotetramers have four identical subunits, and heterotetramers are complexes of different subunits. A tetramer can be assembled as dimer of dimers with two homodimer subunits, or two heterodimer subunits.

Antigen presentation is a vital immune process that is essential for T cell immune response triggering. Because T cells recognize only fragmented antigens displayed on cell surfaces, antigen processing must occur before the antigen fragment, now bound to the major histocompatibility complex (MHC), is transported to the surface of the cell, a process known as presentation, where it can be recognized by a T-cell receptor. If there has been an infection with viruses or bacteria, the cell will present an endogenous or exogenous peptide fragment derived from the antigen by MHC molecules. There are two types of MHC molecules which differ in the behaviour of the antigens: MHC class I molecules (MHC-I) bind peptides from the cell cytosol, while peptides generated in the endocytic vesicles after internalisation are bound to MHC class II (MHC-II). Cellular membranes separate these two cellular environments - intracellular and extracellular. Each T cell can only recognize tens to hundreds of copies of a unique sequence of a single peptide among thousands of other peptides presented on the same cell, because an MHC molecule in one cell can bind to quite a large range of peptides. Predicting which antigens will be presented to the immune system by a certain MHC/HLA type is difficult, but the technology involved is improving.
A tetramer assay is a procedure that uses tetrameric proteins to detect and quantify T cells that are specific for a given antigen within a blood sample. The tetramers used in the assay are made up of four major histocompatibility complex (MHC) molecules, which are found on the surface of most cells in the body. MHC molecules present peptides to T-cells as a way to communicate the presence of viruses, bacteria, cancerous mutations, or other antigens in a cell. If a T-cell's receptor matches the peptide being presented by an MHC molecule, an immune response is triggered. Thus, MHC tetramers that are bioengineered to present a specific peptide can be used to find T-cells with receptors that match that peptide. The tetramers are labeled with a fluorophore, allowing tetramer-bound T-cells to be analyzed with flow cytometry. Quantification and sorting of T-cells by flow cytometry enables researchers to investigate immune response to viral infection and vaccine administration as well as functionality of antigen-specific T-cells. Generally, if a person's immune system has encountered a pathogen, the individual will possess T cells with specificity toward some peptide on that pathogen. Hence, if a tetramer stain specific for a pathogenic peptide results in a positive signal, this may indicate that the person's immune system has encountered and built a response to that pathogen.

Antonio Lanzavecchia is an Italian and Swiss immunologist. As a fellow of Collegio Borromeo he obtained a degree with honors in Medicine in 1976 from the University of Pavia where he specialized in Pediatrics and Infectious Diseases. He is Head Human Immunology Program, Istituto Nazionale di Genetica Molecolare-INGM, Milan and SVP Senior research Fellow, Humabs/Vir Biotechnology, Bellinzona and San Francisco (USA). Since 2017, he is also Professor at the Faculty of Biomedical Sciences of the Università della Svizzera italiana (USI).
HLA class II histocompatibility antigen gamma chain also known as HLA-DR antigens-associated invariant chain or CD74, is a protein that in humans is encoded by the CD74 gene. The invariant chain is a polypeptide which plays a critical role in antigen presentation. It is involved in the formation and transport of MHC class II peptide complexes for the generation of CD4+ T cell responses. The cell surface form of the invariant chain is known as CD74. CD74 is a cell surface receptor for the cytokine macrophage migration inhibitory factor (MIF).

Protein melan-A also known as melanoma antigen recognized by T cells 1 or MART-1 is a protein that in humans is encoded by the MLANA or "MALENA" gene. A fragment of the protein, usually consisting of the nine amino acids 27 to 35, is bound by MHC class I complexes which present it to T cells of the immune system. These complexes can be found on the surface of melanoma cells. Decameric peptides (26-35) are being investigated as cancer vaccines.
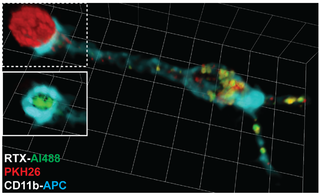
Trogocytosis is when a cell nibbles another cell. It is a process whereby lymphocytes conjugated to antigen-presenting cells extract surface molecules from these cells and express them on their own surface. The molecular reorganization occurring at the interface between the lymphocyte and the antigen-presenting cell during conjugation is also called "immunological synapse".
Immunoevasins are proteins expressed by some viruses that enable the virus to evade immune recognition by interfering with MHC I complexes in the infected cell, therefore blocking the recognition of viral protein fragments by CD8+ cytotoxic T lymphocytes. Less frequently, MHC II antigen presentation and induced-self molecules may also be targeted. Some viral immunoevasins block peptide entry into the endoplasmic reticulum (ER) by targeting the TAP transporters. Immunoevasins are particularly abundant in viruses that are capable of establishing long-term infections of the host, such as herpesviruses.
Immunomics is the study of immune system regulation and response to pathogens using genome-wide approaches. With the rise of genomic and proteomic technologies, scientists have been able to visualize biological networks and infer interrelationships between genes and/or proteins; recently, these technologies have been used to help better understand how the immune system functions and how it is regulated. Two thirds of the genome is active in one or more immune cell types and less than 1% of genes are uniquely expressed in a given type of cell. Therefore, it is critical that the expression patterns of these immune cell types be deciphered in the context of a network, and not as an individual, so that their roles be correctly characterized and related to one another. Defects of the immune system such as autoimmune diseases, immunodeficiency, and malignancies can benefit from genomic insights on pathological processes. For example, analyzing the systematic variation of gene expression can relate these patterns with specific diseases and gene networks important for immune functions.
Immudex is a Danish Reagents and Diagnostics company established in 2009. The company is operating from offices located in Copenhagen, Denmark, and in Fairfax, Virginia. Immudex specializes in the production of MHC Dextramers. MHC Dextramers are chemical reagents that are designed to detect antigen-specific T cells.
Immunodominance is the immunological phenomenon in which immune responses are mounted against only a few of the antigenic peptides out of the many produced. That is, despite multiple allelic variations of MHC molecules and multiple peptides presented on antigen presenting cells, the immune response is skewed to only specific combinations of the two. Immunodominance is evident for both antibody-mediated immunity and cell-mediated immunity. Epitopes that are not targeted or targeted to a lower degree during an immune response are known as subdominant epitopes. The impact of immunodominance is immunodomination, where immunodominant epitopes will curtail immune responses against non-dominant epitopes. Antigen-presenting cells such as dendritic cells, can have up to six different types of MHC molecules for antigen presentation. There is a potential for generation of hundreds to thousands of different peptides from the proteins of pathogens. Yet, the effector cell population that is reactive against the pathogen is dominated by cells that recognize only a certain class of MHC bound to only certain pathogen-derived peptides presented by that MHC class. Antigens from a particular pathogen can be of variable immunogenicity, with the antigen that stimulates the strongest response being the immunodominant one. The different levels of immunogenicity amongst antigens forms what is known as dominance hierarchy.
References
- 1 2 Hadrup, Sine R.; Bakker, Arnold H.; et al. (2009). "Parallel Detection of Antigen-Specific T-Cell responses by multidimensional encoding of MHC multimers". Nature Methods. 6 (7): 520–526. doi:10.1038/nmeth.1345. PMID 19543285. S2CID 1285613.
- ↑ Nepom, Gerald T. "MHC Multimers: Expanding the Clinical Toolkit," Clinical Immunology, Vol 6 (2003), pp. 1-4.,Antigen. 106 (2003), pp. 1-4.
- 1 2 3 Bakker, Arnold; Schumacher, Tom. "MHC Multimer Technology: Current Status and Future Prospects," Current Opinion in Immunology, Vol. 17, No. 4 (August 2005), pp. 428-433.
- 1 2 3 4 5 Nepom, Gerald T (2012). "MHC Class II Tetramers". Journal of Immunology. 188 (6): 2477–2482. doi:10.4049/jimmunol.1102398. PMC 3297979 . PMID 22389204.
- ↑ Holman, Philmore O.; Walsh, Elizabeth R.; Jameson, Stephen C. (2005). "Characterizing the Impact of CD8 Antibodies on Class I MHC Multimer Binding". The Journal of Immunology. 174 (7): 3986–3991. doi: 10.4049/jimmunol.174.7.3986 . PMID 15778355.
- ↑ Hackett, Charles J.; Sharma, Opendra K. (2002). "Frontiers in peptide-MHC class II multimer technology". Nature Immunology. 3 (10): 887–889. doi:10.1038/ni1002-887. PMID 12352960. S2CID 43206855.
- ↑ Davis, Mark M.; Altman, John D.; Newell, Evan W. "Interrogating the Repertoire: Broadening the Scope of Peptide-MHC Multimer Analysis," Nature Reviews Immunology, Vol. 11, No. 8 (July 15, 2011), pp. 551-558.
- ↑ Fairhead, M; Veggiani, G; et al. (2014). "SpyAvidin Hubs Enable Precise and Ultrastable Orthogonal Nanoassembly". Journal of the American Chemical Society. 136 (35): 1528–35. doi:10.1021/ja505584f. PMC 4183622 . PMID 25111182.
- ↑ Erfle V, inventor; 2004 Jul. 15. MHC tetramers. United States patent US 20040137642.
- ↑ Altman, J. D; et al. (1996). "Phenotypic analysis of antigen-specific T lymphocytes". Science. 274 (5284): 94–96. Bibcode:1996Sci...274...94A. doi:10.1126/science.274.5284.94. PMID 8810254. S2CID 12667633.
- ↑ Lebowitz, M. S (1999). "Soluble, high-affinity dimers of T-cell receptors and class II major histocompatibility complexes: biochemical probes for analysis and modulation of immune responses". Cell. Immunol. 192 (2): 175–184. doi: 10.1006/cimm.1999.1441 . PMID 10087186.
- 1 2 3 4 5 Davis, MM; Altman, JD; Newell, EW (Jul 2011). "Interrogating the repertoire: broadening the scope of peptide-MHC multimer analysis". Nat Rev Immunol. 11 (8): 551–8. doi:10.1038/nri3020. PMC 3699324 . PMID 21760610.
- ↑ He, X. S.; et al. (2008). "Phenotypic changes in influenza-specific CD8+ T cells after immunization of children and adults with influenza vaccines". J. Infect. Dis. 197 (6): 803–811. doi: 10.1086/528804 . PMID 18279048.
- ↑ Co, M. D., Kilpatrick, E. D. & Rothman, A. L. Dynamics of the CD8 T-cell response following yellow fever virus 17D immunization" Immunology 2009; 128, e718–e727
- ↑ Wei, H. et al. DR*W201/P65 tetramer visualization of epitope-specific CD4 T-cell during M. tuberculosis infection and its resting memory pool after BCG vaccination" PLoS ONE 4, e6905 (2009).
- ↑ Betts, M. R.; et al. (2005). "Characterization of functional and phenotypic changes in anti-Gag vaccine-induced T cell responses and their role in protection after HIV-1 infection". Proc. Natl. Acad. Sci. USA. 102 (12): 4512–4517. Bibcode:2005PNAS..102.4512B. doi: 10.1073/pnas.0408773102 . PMC 552973 . PMID 15753288.
- ↑ Pittet, M. J.; et al. (2001). "Ex vivo analysis of tumor antigen specific CD8+ T cell responses using MHC/peptide tetramers in cancer patients". Int. Immunopharmacol. 1 (7): 1235–1247. doi:10.1016/s1567-5769(01)00048-0. PMID 11460305.
- ↑ Lee, P. P. et al. Characterization of circulating T cells specific for tumor-associated antigens in melanoma patients.
- ↑ Maile, R.; et al. (2001). "Antigen-specific modulation of an immune response by in vivo administration of soluble MHC class I tetramers". J. Immunol. 167 (7): 3708–3714. doi: 10.4049/jimmunol.167.7.3708 . PMID 11564786.
- ↑ Yuan, R. R.; et al. (2004). "Targeted deletion of T-cell clones using alpha-emitting suicide MHC tetramers". Blood. 104 (8): 2397–2402. doi: 10.1182/blood-2004-01-0324 . PMID 15217835.
- ↑ Cobbold, M.; et al. (2005). "Adoptive transfer of cytomegalovirus-specific CTL to stem cell transplant patients after selection by HLA–peptide tetramers". J. Exp. Med. 202 (3): 379–386. doi:10.1084/jem.20040613. PMC 2213070 . PMID 16061727.
- ↑ Jiang; Clark; Liu; Wagers; Fuhlbrigge; Kupper (2012). "Skin infection generates non-migratory memory CD8+ T(RM) cells providing global skin immunity". Nature. 483 (7388): 227–31. Bibcode:2012Natur.483..227J. doi:10.1038/nature10851. PMC 3437663 . PMID 22388819.
- ↑ Saveanu L, Carroll O, Weimershaus M, Guermonprez P, Firat E, Lindo V, Greer F, Davoust J, Kratzer R, Keller SR, Niedermann G, van Endert P (2009). "IRAP identifies an endosomal compartment required for MHC class I cross-presentation". Science. 325 (5937): 213–7. Bibcode:2009Sci...325..213S. doi:10.1126/science.1172845. PMID 19498108. S2CID 35719774.
- ↑ Bannard; Kraman, Fearon (2009). "Secondary replicative function of CD8+ T cells that had developed an effector phenotype". Science. 323 (5913): 505–9. Bibcode:2009Sci...323..505B. doi:10.1126/science.1166831. PMC 2653633 . PMID 19164749.
- ↑ Panoskaltsis-Mortari; Taylor PA; Riddle MJ; Shlomchik MA; Blazar BR. (2008). "In situ identification of allospecific B cells using pentamers". Blood. 111 (7): 3904–5. doi:10.1182/blood-2007-12-127415. PMC 2275041 . PMID 18362221.
- ↑ Griffioen M, van Egmond HM, Barnby-Porritt H, van der Hoorn MA, Hagedoorn RS, Kester MG, Schwabe N, Willemze R, Falkenburg JH, Heemskerk MH (2008). "Genetic engineering of virus-specific T cells with T-cell receptors recognizing minor histocompatibility antigens for clinical application". Haematologica. 93 (10): 1535–43. doi: 10.3324/haematol.13067 . PMID 18768532.
- ↑ Uhlin; Okas M; Gertow J; Uzunel M; Brismar TB; Mattsson J. (2009). "A novel haplo-identical adoptive CTL therapy as a treatment for EBV-associated lymphoma after stem cell transplantation". Cancer Immunol Immunother. 59 (3): 473–7. doi:10.1007/s00262-009-0789-1. PMID 19908041. S2CID 21605915.
- 1 2 Casalegno-Garduno, Rosaely; Schmitt, Anita; Yao, Junxia; Wang, Xinchao; Xu, Xun; Freund, Mathias; Schmitt, Michael (2010). "Multimer technologies for detection and adoptive transfer of antigen-specific T cells". Cancer Immunol Immunother. 2010 (59): 195–202. doi:10.1007/s00262-009-0778-4. PMID 19847424. S2CID 27882640.
- ↑ Schøller, Jorgen; Singh, Mahavir; Bergmeier, Lesley; Brunstedt, Katja; Wang, Yufei; Whittall, Trevor; Rahman, Durdana; Pido-Lopez, J.; Lehner, T. (2010). "A recombinant human HLA-class I antigen linked to dextran elicits innate and adaptive immune responses". Journal of Immunological Methods. 2010 (360): 1–9. doi:10.1016/j.jim.2010.05.008. PMID 20542039.
- ↑ Batard, Pascal; Peterson, Daniel A.; Devêvre, Estelle; Guillaume, Philippe; Cerottini, Jean-Charles; Rimoldi, Donata; Speiser, Daniel E.; Winther, Lars; Romero, Pedro (2006). "Dextramers: New generation of fluorescent MHC class I/peptide multimers for visualization of antigen-specific CD8+ T cells". Journal of Immunological Methods. 2006 (310): 136–148. doi:10.1016/j.jim.2006.01.006. PMID 16516226.
- ↑ Hadrup SR; Strindhall J; Kollgaard T; et al. "Longitudinal studies of clonally expanded CD8 T cells reveal a repertoire shrinkage predicting mortality and an increased number of dysfunctional cytomegalovirus-specific T cells in the very elderly". Journal of Immunology, 2006, 176(4), 2645–2653
- ↑ Massilamany; et al. "Detection of autoreactive CD4 T cells using major histocompatibility complex class II dextramers". BMC Immunology. 2011 (12): 40.