Thyroid neoplasm is a neoplasm or tumor of the thyroid. It can be a benign tumor such as thyroid adenoma, or it can be a malignant neoplasm, such as papillary, follicular, medullary or anaplastic thyroid cancer. Most patients are 25 to 65 years of age when first diagnosed; women are more affected than men. The estimated number of new cases of thyroid cancer in the United States in 2010 is 44,670 compared to only 1,690 deaths. Of all thyroid nodules discovered, only about 5 percent are cancerous, and under 3 percent of those result in fatalities.
Renal cell carcinoma (RCC) is a kidney cancer that originates in the lining of the proximal convoluted tubule, a part of the very small tubes in the kidney that transport primary urine. RCC is the most common type of kidney cancer in adults, responsible for approximately 90–95% of cases. RCC occurrence shows a male predominance over women with a ratio of 1.5:1. RCC most commonly occurs between 6th and 7th decade of life.

The collecting duct system of the kidney consists of a series of tubules and ducts that physically connect nephrons to a minor calyx or directly to the renal pelvis. The collecting duct system is the last part of nephron and participates in electrolyte and fluid balance through reabsorption and excretion, processes regulated by the hormones aldosterone and vasopressin.

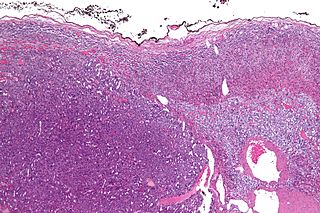
Wilms' tumor or Wilms tumor, also known as nephroblastoma, is a cancer of the kidneys that typically occurs in children, and occurs most commonly as a renal tumor in child patients. It is named after Max Wilms, the German surgeon (1867–1918) who first described it.
Adrenocortical carcinoma (ACC) is an aggressive cancer originating in the cortex of the adrenal gland.
An oncocytoma is a tumor made up of oncocytes, epithelial cells characterized by an excessive amount of mitochondria, resulting in an abundant acidophilic, granular cytoplasm. The cells and the tumor that they compose are often benign but sometimes may be premalignant or malignant.
Malignant rhabdoid tumour (MRT) is a very aggressive form of tumour originally described as a variant of Wilms' tumour, which is primarily a kidney tumour that occurs mainly in children.

Acinic cell carcinoma is a malignant tumor representing 2% of all salivary tumors. 90% of the time found in the parotid gland, 10% intraorally on buccal mucosa or palate. The disease presents as a slow growing mass, associated with pain or tenderness in 50% of the cases. Often appears pseudoencapsulated.

Transitional cell carcinoma, also called urothelial carcinoma, is a type of cancer that typically occurs in the urinary system. It is the most common type of bladder cancer and cancer of the ureter, urethra, and urachus. It accounts for 95% of bladder cancer cases.

A papillary hidradenoma, also termed hidradenoma papilliferum or mammary-like gland adenoma of the vulva, is a rare, but nonetheless most common benign tumor that occurs in and between anal and genital regions of females. These hidradenomas are sharply circumscribed, nodular tumors that usually develop in women's anogenital area but uncommonly occur in other sites in women and men. Papillary hidradenomas that develop outside of the anogenital region are termed ecctopic papillary hidradenomas or ectopic hidradenoma papilliferums.

Proline-rich protein PRCC is a protein that, in humans, is encoded by the PRCC gene.

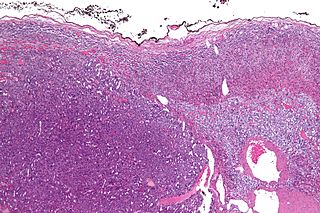
A renal oncocytoma is a tumour of the kidney made up of oncocytes, epithelial cells with an excess amount of mitochondria.
Juxtaglomerular cell tumor is an extremely rare kidney tumour of the juxtaglomerular cells, with less than 100 cases reported in literature. This tumor typically secretes renin, hence the former name of reninoma. It often causes severe hypertension that is difficult to control, in adults and children, although among causes of secondary hypertension it is rare. It develops most commonly in young adults, but can be diagnosed much later in life. It is generally considered benign, but its malignant potential is uncertain.

Kidney tumours are tumours, or growths, on or in the kidney. These growths can be benign or malignant.

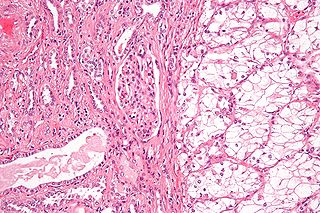
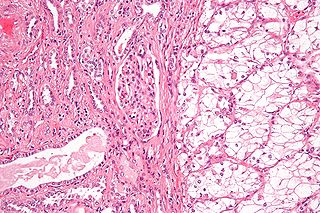
Mucinous tubular and spindle cell carcinoma (MTSCC) is a rare subtype of renal cell carcinoma (RCC), that is included in the 2004 WHO classification of RCC. MTSCC is a rare neoplasm and is considered as a low-grade entity. It may be a variant of papillary RCC. This tumor occurs throughout life and is more frequent in females.

Epithelial-myoepithelial carcinoma (EMCa) is a rare malignant tumour that typically arises in a salivary gland and consists of both an epithelial and myoepithelial component. They are predominantly found in the parotid gland and represent approximately 1% of salivary gland tumours.

Hyalinizing clear cell carcinoma (HCCC) is a rare malignant salivary gland tumour, with a good prognosis, that is usually found on the tongue or palate.
A sialoblastoma is a low-grade salivary gland neoplasm that recapitulates primitive salivary gland anlage. It has previously been referred to as congenital basal cell adenoma, embryoma, or basaloid adenocarcinoma. It is an extremely rare tumor, with less than 100 cases reported worldwide.

An endolymphatic sac tumor (ELST) is a very uncommon papillary epithelial neoplasm arising within the endolymphatic sac or endolymphatic duct. This tumor shows a very high association with Von Hippel–Lindau syndrome (VHL).

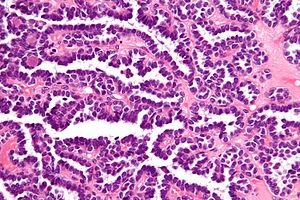
Papillary renal cell carcinoma (PRCC) is a malignant, heterogeneous tumor originating from renal tubular epithelial cells of the kidney, which comprises approximately 10-15% of all kidney neoplasms. Based on its morphological features, PRCC can be classified into two main subtypes, which are type 1 (basophilic) and type 2 (eosinophilic).