Related Research Articles

Interventional radiology (IR) is a medical specialty that performs various minimally-invasive procedures using medical imaging guidance, such as x-ray fluoroscopy, computed tomography, magnetic resonance imaging, or ultrasound. IR performs both diagnostic and therapeutic procedures through very small incisions or body orifices. Diagnostic IR procedures are those intended to help make a diagnosis or guide further medical treatment, and include image-guided biopsy of a tumor or injection of an imaging contrast agent into a hollow structure, such as a blood vessel or a duct. By contrast, therapeutic IR procedures provide direct treatment—they include catheter-based medicine delivery, medical device placement, and angioplasty of narrowed structures.

Vascular surgery is a surgical subspecialty in which vascular diseases involving the arteries, veins, or lymphatic vessels, are managed by medical therapy, minimally-invasive catheter procedures and surgical reconstruction. The specialty evolved from general and cardiovascular surgery where it refined the management of just the vessels, no longer treating the heart or other organs. Modern vascular surgery includes open surgery techniques, endovascular techniques and medical management of vascular diseases - unlike the parent specialities. The vascular surgeon is trained in the diagnosis and management of diseases affecting all parts of the vascular system excluding the coronaries and intracranial vasculature. Vascular surgeons also are called to assist other physicians to carry out surgery near vessels, or to salvage vascular injuries that include hemorrhage control, dissection, occlusion or simply for safe exposure of vascular structures.

An aortic aneurysm is an enlargement (dilatation) of the aorta to greater than 1.5 times normal size. They usually cause no symptoms except when ruptured. Occasionally, there may be abdominal, back, or leg pain. The prevalence of abdominal aortic aneurysm ("AAA") has been reported to range from 2 to 12% and is found in about 8% of men more than 65 years of age. The mortality rate attributable to AAA is about 15,000 per year in the United States and 6,000 to 8,000 per year in the United Kingdom and Ireland. Between 2001 and 2006, there were approximately 230,000 AAA surgical repairs performed on Medicare patients in the United States.

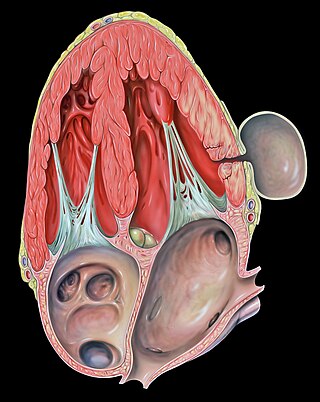
Abdominal aortic aneurysm (AAA) is a localized enlargement of the abdominal aorta such that the diameter is greater than 3 cm or more than 50% larger than normal. An AAA usually causes no symptoms, except during rupture. Occasionally, abdominal, back, or leg pain may occur. Large aneurysms can sometimes be felt by pushing on the abdomen. Rupture may result in pain in the abdomen or back, low blood pressure, or loss of consciousness, and often results in death.
A pseudoaneurysm, also known as a false aneurysm, is a locally contained hematoma outside an artery or the heart due to damage to the vessel wall. The injury passes through all three layers of the arterial wall, causing a leak, which is contained by a new, weak "wall" formed by the products of the clotting cascade. A pseudoaneurysm does not contain any layer of the vessel wall.

Traumatic aortic rupture, also called traumatic aortic disruption or transection, is a condition in which the aorta, the largest artery in the body, is torn or ruptured as a result of trauma to the body. The condition is frequently fatal due to the profuse bleeding that results from the rupture. Since the aorta branches directly from the heart to supply blood to the rest of the body, the pressure within it is very great, and blood may be pumped out of a tear in the blood vessel very rapidly. This can quickly result in shock and death. Thus traumatic aortic rupture is a common killer in automotive accidents and other traumas, with up to 18% of deaths that occur in automobile collisions being related to the injury. In fact, aortic disruption due to blunt chest trauma is the second leading cause of injury death behind traumatic brain injury.

Endovascular aneurysm repair (EVAR) is a type of minimally-invasive endovascular surgery used to treat pathology of the aorta, most commonly an abdominal aortic aneurysm (AAA). When used to treat thoracic aortic disease, the procedure is then specifically termed TEVAR for "thoracic endovascular aortic/aneurysm repair." EVAR involves the placement of an expandable stent graft within the aorta to treat aortic disease without operating directly on the aorta. In 2003, EVAR surpassed open aortic surgery as the most common technique for repair of AAA, and in 2010, EVAR accounted for 78% of all intact AAA repair in the United States.

Randall Bertram Griepp was an American cardiothoracic surgeon who collaborated with Norman Shumway in the development of the first successful heart transplant procedures in the U.S. He had an international reputation for contributions to the surgical treatment of aortic aneurysms and aortic dissection and in heart and lung transplantations. He received nearly $8 million in grants from the National Heart, Lung, and Blood Institute.

Peter Lin is an American vascular surgeon, medical researcher, specializing in minimally invasive endovascular treatment of vascular disease. He has published extensively in the area of vascular surgery and endovascular surgery.
Surgical Outcomes Analysis & Research, SOAR, is a research laboratory of the Department of Surgery at Boston University School of Medicine and Boston Medical Center with expertise in outcomes research. SOAR investigates surgical diseases and perioperative outcomes. The group focuses on pancreatic cancer, other gastrointestinal and hepatobiliary malignancies, vascular disease, and transplant surgery. SOAR's goal is to examine quality, delivery, and financing of care in order to have an immediate impact on patient care and system improvements. The group members utilize national health services and administrative databases, as well as institutional databases, to investigate and to address factors contributing to disease outcomes and healthcare disparities.

A hybrid cardiac surgical procedure in a narrow sense is defined as a procedure that combines a conventional, more invasive surgical part with an interventional part, using some sort of catheter-based procedure guided by fluoroscopy imaging in a hybrid operating room (OR) without interruption. The hybrid technique has a reduced risk of surgical complications and has shown decreased recovery time. It can be used to treat numerous heart diseases and conditions and with the increasing complexity of each case, the hybrid surgical technique is becoming more common.

Open aortic surgery (OAS), also known as open aortic repair (OAR), describes a technique whereby an abdominal, thoracic or retroperitoneal surgical incision is used to visualize and control the aorta for purposes of treatment, usually by the replacement of the affected segment with a prosthetic graft. OAS is used to treat aneurysms of the abdominal and thoracic aorta, aortic dissection, acute aortic syndrome, and aortic ruptures. Aortobifemoral bypass is also used to treat atherosclerotic disease of the abdominal aorta below the level of the renal arteries. In 2003, OAS was surpassed by endovascular aneurysm repair (EVAR) as the most common technique for repairing abdominal aortic aneurysms in the United States.
Frank J. Veith is an American vascular surgeon who serves as Professor of Surgery, New York University Medical Center NY, NY and Professor of Surgery Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, Cleveland, OH. He was the first vascular surgeon in the United States to perform minimally invasive aortic aneurysm surgery together with Drs. Michael L. Marin, Juan C. Parodi and Claudio J. Schonholz.
Juan Carlos Parodi is an Argentinian vascular surgeon who introduced the minimally invasive endovascular aneurysm repair (EVAR) to the world and performed the first successful endovascular repair of an abdominal aortic aneurysm on 7 September 1990 in Buenos Aires. In 1992 he was the first in the United States to perform minimally invasive aortic aneurysm surgery together with Drs. Frank Veith, Michael L. Marin and Claudio J. Schonholz. He continues to develop new techniques, including seat belt and air bag technique for cerebral protection during carotid stenting. He is recognized as a renowned pioneer in the specialty of endovascular repairs of the aorta.
Claudio J. Schonholz is an interventional radiologist, the first in the United States to perform minimally invasive aortic aneurysm surgery together with Drs. Frank Veith, Juan C. Parodi and Michael L. Marin.
Endovascular and hybrid trauma and bleeding management is a new and rapidly evolving concept within medical healthcare and endovascular resuscitation. It involves early multidisciplinary evaluation and management of hemodynamically unstable patients with traumatic injuries as well as being a bridge to definitive treatment. It has recently been shown that the EVTM concept may also be applied to non-traumatic hemodynamically unstable patients.

Nicolai Leontievich Volodos, was a Soviet/Ukrainian cardiovascular surgeon and scientist. An innovator, Volodos developed and introduced into clinical practice the world's first endovascular stent graft for the treatment of stenotic and aneurysmal diseases of arterial system. Volodos was described by his colleagues as ”a pioneer innovator and a giant in vascular and endovascular surgery” and ”a giant of historic proportions in the vascular and endovascular specialties, and the father of endovascular grafting”.
Gustavo S. Oderich is a Brazilian American vascular and endovascular surgeon who serves as a professor and chief of vascular and endovascular surgery, and is the director of the Advanced Endovascular Aortic Program at McGovern Medical School at The University of Texas Health Science Center at Houston and Memorial Hermann Health System. He previously served as chair of vascular and endovascular division at the Mayo Clinic in Rochester, Minnesota. Oderich is recognized for his work in minimally invasive endovascular surgery and research in fenestrated and branched stent-graft technology to treat complex aortic aneurysms and dissections.

Benjamin Starnes is a vascular surgeon and medical researcher. He holds the Alexander Whitehill Clowes Endowed Chair in Vascular surgery at the University of Washington. He served as a U.S. Army surgeon for 15 years, doing three tours of duty, including in the last M.A.S.H. unit. On the day of the September 11 attacks he was at the Pentagon rendering medical aid to victims, and his experience was later recounted in the book American Phoenix: Heroes of the Pentagon on 9/11. He is among the primary authors of the official guidelines for diagnosis and management of aortic disease adopted by the American College of Cardiology and the American Heart Association.
Isolated superior mesenteric artery dissection (ISMAD) is a rare but potentially life-threatening condition that causes acute abdominal pain. It refers to a dissection that occurs solely in the superior mesenteric artery (SMA), typically spontaneously, and does not involve the aorta. Although aortic dissection can frequently extend into its peripheral territories, it is rare for these branches to have dissection without main aortic trunk involvement. The SMA is the most common site of dissection among visceral arteries compared to other gastrointestinal arteries.
References
- ↑ Veith, Frank J; Marin, Michael M; Cynamon, Jacob; Schonholz, Claudio; Parodi, Juan (2005). "1992: Parodi, Montefiore, and the First Abdominal Aortic Aneurysm Stent Graft in the United States". Annals of Vascular Surgery. 19 (5): 749–751. doi:10.1007/s10016-005-6858-9. ISSN 0890-5096. PMID 16052384. S2CID 36486311.
- ↑ "Claudio Schonholz, M.D." Medical University of South Carolina. Retrieved September 21, 2019.
- ↑ "Best Doctors 2004 - Vascular Surgery Innovator - Michael Marin - Nymag". New York Magazine. Retrieved May 21, 2020.
- 1 2 "Michael L. Marin, MD FACS". American College of Surgeons. Archived from the original on September 21, 2019. Retrieved July 29, 2023.
- ↑ "Dr. Michael Marin, MD – New York, NY | Vascular Surgery on Doximity". Doximity. Retrieved May 21, 2020.
- ↑ "Michael L. Marin, MD – NY Endovascular Summit" . Retrieved May 21, 2020.
- ↑ "Chair Message". Mount Sinai School of Medicine. Retrieved September 21, 2019.
- ↑ HITInfrastructure (April 15, 2019). "Mount Sinai Gets $6M for Center with New Health IT Infrastructure". HITInfrastructure. Retrieved May 21, 2020.
- ↑ "Dr. Michael Marin helps build ASC in rural Uganda village — 4 key notes". Becker's ASC Review. Retrieved September 21, 2019.
- ↑ Raskin, Laura (July 5, 2017). "Kyabirwa Ambulatory Surgery Center by Kliment Halsband Architects". Architectural Record. Retrieved September 21, 2019.
- ↑ Hoffman, Jan (March 25, 2017). "Going Under the Knife, With Eyes and Ears Wide Open". The New York Times. Bensalem, Pennsylvania. Retrieved July 29, 2023.
- ↑ "US Patent for Method and apparatus concerning bypass grafts Patent (Patent # 6,575,994 issued June 10, 2003) - Justia Patents Search". patents.justia.com. Retrieved May 21, 2020.
- ↑ "US Patent for Method for endoluminal excluding an aortic aneurysm Patent (Patent # 6,168,610 issued January 2, 2001) - Justia Patents Search". patents.justia.com. Retrieved May 21, 2020.
- ↑ "US Patent for Method and apparatus for deploying non-circular stents and graft stent complexes Patent (Patent # 6,039,749 issued March 21, 2000) - Justia Patents Search". patents.justia.com. Retrieved May 21, 2020.
- ↑ Falchuk, Ben (December 7, 2010), "Deploying Intelligent Mobile Applications", Mobile Web 2.0, Auerbach Publications, pp. 237–263, doi:10.1201/b10445-12, ISBN 978-1-4398-0082-9
- ↑ "US Patent for Method and apparatus for forming an endoluminal bifurcated graft Patent (Patent # 5,695,517 issued December 9, 1997) - Justia Patents Search". patents.justia.com. Retrieved May 21, 2020.
- ↑ "US Patent for Apparatus and method for deployment of radially expandable stents by a mechanical linkage Patent (Patent # 5,618,300 issued April 8, 1997) - Justia Patents Search". patents.justia.com. Retrieved May 21, 2020.
- ↑ "US Patent for Method for the deployment of radially expandable stents Patent (Patent # 5,591,196 issued January 7, 1997) - Justia Patents Search". patents.justia.com. Retrieved May 21, 2020.
- ↑ "US Patent for Method for delivering and deploying intraluminal devices Patent (Patent # 5,569,296 issued October 29, 1996) - Justia Patents Search". patents.justia.com. Retrieved May 21, 2020.
- ↑ "US Patent for Method and apparatus for forming an endoluminal bifurcated graft Patent (Patent # 5,507,769 issued April 16, 1996) - Justia Patents Search". patents.justia.com. Retrieved May 21, 2020.
- ↑ "US Patent for Device for delivering and deploying intraluminal devices Patent (Patent # 5,456,694 issued October 10, 1995) - Justia Patents Search". patents.justia.com. Retrieved May 21, 2020.
- ↑ "US Patent for Apparatus and method for deployment of radially expandable stents by a mechanical linkage Patent (Patent # 5,443,477 issued August 22, 1995) - Justia Patents Search". patents.justia.com. Retrieved May 21, 2020.
- ↑ "US Patent for Intraluminal stent Patent (Patent # 5,397,355 issued March 14, 1995) - Justia Patents Search". patents.justia.com. Retrieved May 21, 2020.