Cerebrospinal fluid (CSF) is a clear, colorless body fluid found within the tissue that surrounds the brain and spinal cord of all vertebrates.

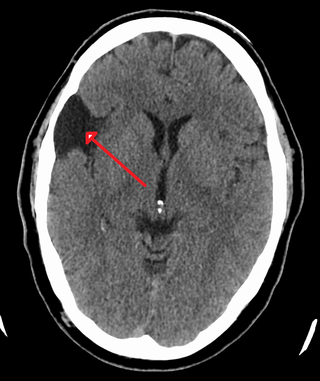
A brain tumor occurs when abnormal cells form within the brain. There are two main types of tumors: malignant tumors and benign (non-cancerous) tumors. These can be further classified as primary tumors, which start within the brain, and secondary tumors, which most commonly have spread from tumors located outside the brain, known as brain metastasis tumors. All types of brain tumors may produce symptoms that vary depending on the size of the tumor and the part of the brain that is involved. Where symptoms exist, they may include headaches, seizures, problems with vision, vomiting and mental changes. Other symptoms may include difficulty walking, speaking, with sensations, or unconsciousness.

The choroid plexus, or plica choroidea, is a plexus of cells that arises from the tela choroidea in each of the ventricles of the brain. Regions of the choroid plexus produce and secrete most of the cerebrospinal fluid (CSF) of the central nervous system. The choroid plexus consists of modified ependymal cells surrounding a core of capillaries and loose connective tissue. Multiple cilia on the ependymal cells move to circulate the cerebrospinal fluid.

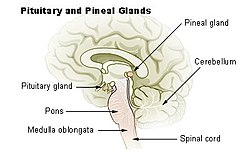
Pinealocytes are the main cells contained in the pineal gland, located behind the third ventricle and between the two hemispheres of the brain. The primary function of the pinealocytes is the secretion of the hormone melatonin, important in the regulation of circadian rhythms. In humans, the suprachiasmatic nucleus of the hypothalamus communicates the message of darkness to the pinealocytes, and as a result, controls the day and night cycle. It has been suggested that pinealocytes are derived from photoreceptor cells. Research has also shown the decline in the number of pinealocytes by way of apoptosis as the age of the organism increases. There are two different types of pinealocytes, type I and type II, which have been classified based on certain properties including shape, presence or absence of infolding of the nuclear envelope, and composition of the cytoplasm.

An ependymoma is a tumor that arises from the ependyma, a tissue of the central nervous system. Usually, in pediatric cases the location is intracranial, while in adults it is spinal. The common location of intracranial ependymomas is the fourth ventricle. Rarely, ependymomas can occur in the pelvic cavity.

A pinealoma is a tumor of the pineal gland, a part of the brain that produces melatonin. If a pinealoma destroys the cells of the pineal gland in a child, it can cause precocious puberty.

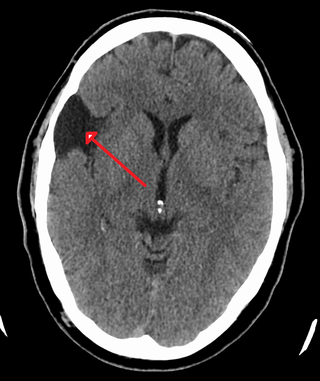
Choroid plexus papilloma, also known as papilloma of the choroid plexus, is a rare benign neuroepithelial intraventricular WHO grade I lesion found in the choroid plexus. It leads to increased cerebrospinal fluid production, thus causing increased intracranial pressure and hydrocephalus.

A papillary hidradenoma, also termed hidradenoma papilliferum or mammary-like gland adenoma of the vulva, is a rare, but nonetheless most common benign tumor that occurs in and between anal and genital regions of females. These hidradenomas are sharply circumscribed, nodular tumors that usually develop in women's anogenital area but uncommonly occur in other sites in women and men. Papillary hidradenomas that develop outside of the anogenital region are termed ecctopic papillary hidradenomas or ectopic hidradenoma papilliferums.

The subcommissural organ (SCO) is one of the circumventricular organs of the brain. It is a small glandular structure that is located in the posterior region of the third ventricle, near the entrance of the cerebral aqueduct.

An atypical teratoid rhabdoid tumor (AT/RT) is a rare tumor usually diagnosed in childhood. Although usually a brain tumor, AT/RT can occur anywhere in the central nervous system (CNS), including the spinal cord. About 60% will be in the posterior cranial fossa. One review estimated 52% in the posterior fossa, 39% are supratentorial primitive neuroectodermal tumors (sPNET), 5% are in the pineal, 2% are spinal, and 2% are multifocal.
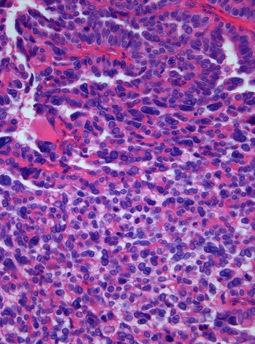
Choroid plexus tumors are a rare type of cancer that occur from the brain tissue called choroid plexus of the brain. Choroid plexus tumors are uncommon tumors of the central nervous system that account for 0.5–0.6% of intracranial neoplasms in people of all ages. Choroid plexus papilloma, atypical choroid plexus papilloma, and choroid plexus carcinoma are the three World Health Organization grades for these cancers, respectively. Children under the age of five account for 10% of cases of choroid plexus tumors. In children and adults, respectively, the lateral ventricle and the fourth ventricle are common locations, About 5% of all choroid plexus tumors are located in the third ventricle. Along with other unusual places such the cerebellopontine angle, the Luschka foramen, or brain parenchyma, the third ventricle is a rare location for choroid plexus tumors. Together, atypical choroid plexus papilloma, and choroid plexus carcinoma make up around 25% of all choroid plexus tumors. Although there have been reports of third ventricle choroid plexus papillomas in people in their fifth decade of life, only 14% of choroid plexus tumors are reported to arise in infants. Most findings indicate that choroid plexus tumors have no sex predilection.

Gliosarcoma is a rare type of glioma, a cancer of the brain that comes from glial, or supportive, brain cells, as opposed to the neural brain cells. Gliosarcoma is a malignant cancer, and is defined as a glioblastoma consisting of gliomatous and sarcomatous components. Primary gliosarcoma (PGS) is classified as a grade IV tumor and a subtype of glioblastoma multiforme in the 2007 World Health Organization classification system (GBM). Because of a lack of specific and clear diagnostic criteria, the word "gliosarcoma" was frequently used to refer to glial tumours with mesenchymal properties, such as the ability to make collagen and reticulin.

Leptomeningeal cancer is a rare complication of cancer in which the disease spreads from the original tumor site to the meninges surrounding the brain and spinal cord. This leads to an inflammatory response, hence the alternative names neoplastic meningitis (NM), malignant meningitis, or carcinomatous meningitis. The term leptomeningeal describes the thin meninges, the arachnoid and the pia mater, between which the cerebrospinal fluid is located. The disorder was originally reported by Eberth in 1870. It is also known as leptomeningeal carcinomatosis, leptomeningeal disease (LMD), leptomeningeal metastasis, meningeal metastasis and meningeal carcinomatosis.
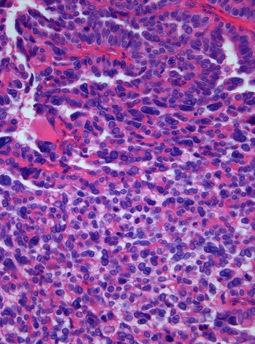
A choroid plexus carcinoma is a type of choroid plexus tumor that affects the choroid plexus of the brain. It is considered the worst of the three grades of chord plexus tumors, having a much poorer prognosis than choroid atypical plexus papilloma and choroid plexus papilloma. The disease creates lesions in the brain and increases cerebrospinal fluid volume, resulting in hydrocephalus.
A central nervous system cyst is a type of cyst that presents and affects part of the central nervous system (CNS). They are usually benign and filled with either cerebrospinal fluid, blood, or tumor cells. CNS cysts are classified into two categories: cysts that originate from non-central nervous system tissue, migrate to, and form on a portion of the CNS, and cysts that originate within central nervous system tissue itself. Within these two categories, there are many types of CNS cysts that have been identified from previous studies.

Pineoblastoma is a malignant tumor of the pineal gland. A pineoblastoma is a supratentorial midline primitive neuroectodermal tumor. Pineoblastoma can present at any age, but is most common in young children. They account for 0.001% of all primary CNS neoplasms.

The following is a simplified (deprecated) version of the 2021 WHO classification of the tumours of the central nervous system. Currently, as of 2021, clinicians are using the WHO grade 5th edition, which incorporates recent advances in molecular pathology.

An endolymphatic sac tumor (ELST) is a very uncommon papillary epithelial neoplasm arising within the endolymphatic sac or endolymphatic duct. This tumor shows a very high association with Von Hippel–Lindau syndrome (VHL).

Angiocentric glioma (AG) refers to a rare neuroepithelial tumor when the superficial brain malignant cells enclose the brain vessels, commonly found in children and young adults. Initially identified in 2005 by Wang and his team from the University of Texas, AG was classified as Grade I by 2007 WHO Classification of Tumors of the Central Nervous System due to its benign clinical behavior, low proliferation index, and curative properties. AG primarily affects children and young adults at an average initial diagnosis age of 16 years old. Over 85% AG patients experience intractable seizures since childhood, especially partial epilepsy.
Mammary secretory carcinoma (MSC), also termed secretory carcinoma of the breast, is a rare form of the breast cancers. MSC usually affects women but in a significant percentage of cases also occurs in men and children. Indeed, McDvitt and Stewart first described MSC in 1966 and termed it juvenile breast carcinoma because an increased number of cases were at that time diagnosed in juvenile females. MSC is the most common form of breast cancer in children, representing 80% of childhood breast cancers, although it accounts for less than 0.15% of all breast cancers.