Cerebrospinal fluid (CSF) is a clear, colorless body fluid found within the tissue that surrounds the brain and spinal cord of all vertebrates.

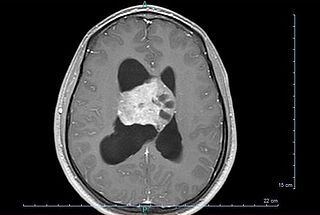
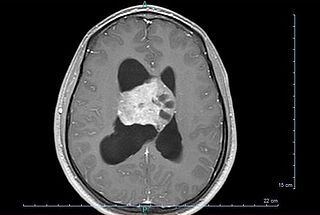
Hydrocephalus is a condition in which an accumulation of cerebrospinal fluid (CSF) occurs within the brain. This typically causes increased pressure inside the skull. Older people may have headaches, double vision, poor balance, urinary incontinence, personality changes, or mental impairment. In babies, it may be seen as a rapid increase in head size. Other symptoms may include vomiting, sleepiness, seizures, and downward pointing of the eyes.

Intracranial pressure (ICP) is the pressure exerted by fluids such as cerebrospinal fluid (CSF) inside the skull and on the brain tissue. ICP is measured in millimeters of mercury (mmHg) and at rest, is normally 7–15 mmHg for a supine adult. The body has various mechanisms by which it keeps the ICP stable, with CSF pressures varying by about 1 mmHg in normal adults through shifts in production and absorption of CSF.

The choroid plexus, or plica choroidea, is a plexus of cells that arises from the tela choroidea in each of the ventricles of the brain. Regions of the choroid plexus produce and secrete most of the cerebrospinal fluid (CSF) of the central nervous system. The choroid plexus consists of modified ependymal cells surrounding a core of capillaries and loose connective tissue. Multiple cilia on the ependymal cells move to circulate the cerebrospinal fluid.

An ependymoma is a tumor that arises from the ependyma, a tissue of the central nervous system. Usually, in pediatric cases the location is intracranial, while in adults it is spinal. The common location of intracranial ependymomas is the fourth ventricle. Rarely, ependymomas can occur in the pelvic cavity.

Choroid plexus cysts (CPCs) are cysts that occur within choroid plexus of the brain. They are the most common type of intraventricular cyst, occurring in 1% of all pregnancies.

The lateral ventricles are the two largest ventricles of the brain and contain cerebrospinal fluid (CSF). Each cerebral hemisphere contains a lateral ventricle, known as the left or right lateral ventricle, respectively.

A colloid cyst is a non-malignant tumor in the brain. It consists of a gelatinous material contained within a membrane of epithelial tissue. It is almost always found just posterior to the foramen of Monro in the anterior aspect of the third ventricle, originating from the roof of the ventricle. Because of its location, it can cause obstructive hydrocephalus and increased intracranial pressure. Colloid cysts represent 0.5–1.0% of intracranial tumors.

A cerebral shunt is a device permanently implanted inside the head and body to drain excess fluid away from the brain. They are commonly used to treat hydrocephalus, the swelling of the brain due to excess buildup of cerebrospinal fluid (CSF). If left unchecked, the excess CSF can lead to an increase in intracranial pressure (ICP), which can cause intracranial hematoma, cerebral edema, crushed brain tissue or herniation. The drainage provided by a shunt can alleviate or prevent these problems in patients with hydrocephalus or related diseases.

Intraventricular hemorrhage (IVH), also known as intraventricular bleeding, is a bleeding into the brain's ventricular system, where the cerebrospinal fluid is produced and circulates through towards the subarachnoid space. It can result from physical trauma or from hemorrhagic stroke.
Endoscopic third ventriculostomy (ETV) is a surgical procedure for treatment of hydrocephalus in which an opening is created in the floor of the third ventricle using an endoscope placed within the ventricular system through a burr hole. This allows the cerebrospinal fluid to flow directly to the basal cisterns, bypassing the obstruction. Specifically, the opening is created in the translucent tuber cinereum on the third ventricular floor.
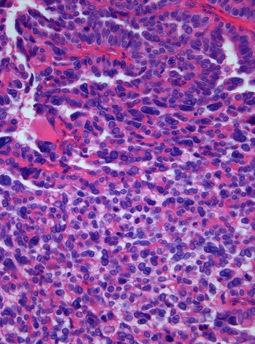
Choroid plexus tumors are a rare type of cancer that occur from the brain tissue called choroid plexus of the brain. Choroid plexus tumors are uncommon tumors of the central nervous system that account for 0.5–0.6% of intracranial neoplasms in people of all ages. Choroid plexus papilloma, atypical choroid plexus papilloma, and choroid plexus carcinoma are the three World Health Organization types for these neoplasms. Children under the age of five account for 10% of cases of choroid plexus tumors. In children and adults, respectively, the lateral ventricle and the fourth ventricle are common locations, About 5% of all choroid plexus tumors are located in the third ventricle. Along with other unusual places such the cerebellopontine angle, the Luschka foramen, or brain parenchyma, the third ventricle is a rare location for choroid plexus tumors. Together, atypical choroid plexus papilloma, and choroid plexus carcinoma make up around 25% of all choroid plexus tumors. Although there have been reports of third ventricle choroid plexus papillomas in people in their fifth decade of life, only 14% of choroid plexus tumors are reported to arise in infants. Most findings indicate that choroid plexus tumors have no sex predilection.
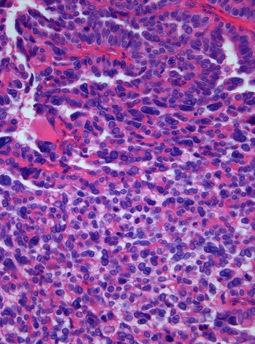
A choroid plexus carcinoma is a type of choroid plexus tumor that affects the choroid plexus of the brain. It is considered the worst of the three grades of chord plexus tumors, having a much poorer prognosis than choroid atypical plexus papilloma and choroid plexus papilloma. The disease creates lesions in the brain and increases cerebrospinal fluid volume, resulting in hydrocephalus.
Bobble-head doll syndrome is a rare neurological movement disorder in which patients, usually children around age 3, begin to bob their head and shoulders forward and back, or sometimes side-to-side, involuntarily, in a manner reminiscent of a bobblehead doll. The syndrome is related to cystic lesions and swelling of the third ventricle in the brain.

Medulloepithelioma is a rare, primitive, fast-growing brain tumour thought to stem from cells of the embryonic medullary cavity. Tumours originating in the ciliary body of the eye are referred to as embryonal medulloepitheliomas, or diktyomas.

Astroblastoma is a rare glial tumor derived from the astroblast, a type of cell that closely resembles spongioblastoma and astrocytes. Astroblastoma cells are most likely found in the supratentorial region of the brain that houses the cerebrum, an area responsible for all voluntary movements in the body. It also occurs significantly in the frontal lobe, parietal lobe, and temporal lobe, areas where movement, language creation, memory perception, and environmental surroundings are expressed. These tumors can be present in major brain areas not associated with the main cerebral hemispheres, including the cerebellum, optic nerve, cauda equina, hypothalamus, and brain stem.

Papillary tumors of the pineal region were first described by A. Jouvet et al. in 2003 and were introduced in the World Health Organization (WHO) classification of central nervous system in 2007. Papillary Tumors of the Pineal Region are located on the pineal gland which is located in the center of the brain. The pineal gland is located on roof of the diencephalon. It is a cone-shaped structure dorsal to the midbrain tectum. The tumor appears to be derived from the specialized ependymal cells of the subcommissural organ. Papillary tumors of the central nervous system and particularly of the pineal region are very rare and so diagnosing them is extremely difficult.
Central neurocytoma (CNC) is an extremely rare, ordinarily benign intraventricular brain tumour that typically forms from the neuronal cells of the septum pellucidum. The majority of central neurocytomas grow inwards into the ventricular system forming interventricular neurocytomas. This leads to two primary symptoms of CNCs, blurred vision and increased intracranial pressure. Treatment for a central neurocytoma typically involves surgical removal, with an approximate 1 in 5 chance of recurrence. Central neurocytomas are classified as a grade II tumor under the World Health Organization's classification of tumors of the nervous system.

Angiocentric glioma (AG) refers to a rare neuroepithelial tumor when the superficial brain malignant cells enclose the brain vessels, commonly found in children and young adults. Initially identified in 2005 by Wang and his team from the University of Texas, AG was classified as Grade I by 2007 WHO Classification of Tumors of the Central Nervous System due to its benign clinical behavior, low proliferation index, and curative properties. AG primarily affects children and young adults at an average initial diagnosis age of 16 years old. Over 85% AG patients experience intractable seizures since childhood, especially partial epilepsy.
Diffuse leptomeningeal glioneuronal tumor (DLGNT) is a rare, primary CNS tumor, classified as distinct entity in 2016 and described as diffuse oligodendroglial-like leptomeningeal tumor of children in the 2016 classification of CNS neoplasms by the WHO., Typically, it's considered juvenile tumors but can occur in adults, the average age of diagnosis is five years. It's characterised by wide leptomeningeal spread with male predominance, like histopathology of neurocytoma, oligodendrocyte-like cytopathology, bland appearance, and severe clinical behaviour. Children's basal cisterns and inter-hemispheric fissures are typically involved in plaque like subarachnoid tumors. A common related intraparenchymal lesion is a spinal lesion. However, in certain situations, superficial parenchyma or Virchow-Robin gaps were affected.
Molecular and genetic investigations frequently show a combination of KIAA1549 and the serine/threonine protein kinase BRAF gene, and also deletions of the short arm of chromosome number 1 and/or the long arm of chromosome number 19.