
Encephalitis is inflammation of the brain. The severity can be variable with symptoms including reduction or alteration in consciousness, headache, fever, confusion, a stiff neck, and vomiting. Complications may include seizures, hallucinations, trouble speaking, memory problems, and problems with hearing.

Viral meningitis, also known as aseptic meningitis, is a type of meningitis due to a viral infection. It results in inflammation of the meninges. Symptoms commonly include headache, fever, sensitivity to light and neck stiffness.

Shingles, also known as herpes zoster, is a viral disease characterized by a painful skin rash with blisters in a localized area. Typically the rash occurs in a single, wide mark either on the left or right side of the body or face. Two to four days before the rash occurs there may be tingling or local pain in the area. Other common symptoms are fever, headache, and tiredness. The rash usually heals within two to four weeks, but some people develop ongoing nerve pain which can last for months or years, a condition called postherpetic neuralgia (PHN). In those with poor immune function the rash may occur widely. If the rash involves the eye, vision loss may occur.

Arbovirus is an informal name for any virus that is transmitted by arthropod vectors. The term arbovirus is a portmanteau word. Tibovirus is sometimes used to more specifically describe viruses transmitted by ticks, a superorder within the arthropods. Arboviruses can affect both animals and plants. In humans, symptoms of arbovirus infection generally occur 3–15 days after exposure to the virus and last three or four days. The most common clinical features of infection are fever, headache, and malaise, but encephalitis and viral hemorrhagic fever may also occur.
La Crosse encephalitis is an encephalitis caused by an arbovirus which has a mosquito vector.

Aseptic meningitis is the inflammation of the meninges, a membrane covering the brain and spinal cord, in patients whose cerebral spinal fluid test result is negative with routine bacterial cultures. Aseptic meningitis is caused by viruses, mycobacteria, spirochetes, fungi, medications, and cancer malignancies. The testing for both meningitis and aseptic meningitis is mostly the same. A cerebrospinal fluid sample is taken by lumbar puncture and is tested for leukocyte levels to determine if there is an infection and goes on to further testing to see what the actual cause is. The symptoms are the same for both meningitis and aseptic meningitis but the severity of the symptoms and the treatment can depend on the certain cause.

Gingivostomatitis is a combination of gingivitis and stomatitis, or an inflammation of the oral mucosa and gingiva. Herpetic gingivostomatitis is often the initial presentation during the first ("primary") herpes simplex infection. It is of greater severity than herpes labialis which is often the subsequent presentations. Primary herpetic gingivostomatitis is the most common viral infection of the mouth.

Meningoencephalitis, also known as herpes meningoencephalitis, is a medical condition that simultaneously resembles both meningitis, which is an infection or inflammation of the meninges, and encephalitis, which is an infection or inflammation of the brain tissue.

Genital herpes is a herpes infection of the genitals caused by the herpes simplex virus (HSV). Most people either have no or mild symptoms and thus do not know they are infected. When symptoms do occur, they typically include small blisters that break open to form painful ulcers. Flu-like symptoms, such as fever, aching, or swollen lymph nodes, may also occur. Onset is typically around 4 days after exposure with symptoms lasting up to 4 weeks. Once infected further outbreaks may occur but are generally milder.

Mollaret's meningitis is a recurrent or chronic inflammation of the protective membranes covering the brain and spinal cord, known collectively as the meninges. Since Mollaret's meningitis is a recurrent, benign (non-cancerous), aseptic meningitis, it is also referred to as benign recurrent lymphocytic meningitis. It was named for Pierre Mollaret, the French neurologist who first described it in 1944.
The central nervous system (CNS) controls most of the functions of the body and mind. It comprises the brain, spinal cord and the nerve fibers that branch off to all parts of the body. The CNS viral diseases are caused by viruses that attack the CNS. Existing and emerging viral CNS infections are major sources of human morbidity and mortality.

Mosquito-borne diseases or mosquito-borne illnesses are diseases caused by bacteria, viruses or parasites transmitted by mosquitoes. Nearly 700 million people contract mosquito-borne illnesses each year, resulting in more than a million deaths.

Herpes simplex, often known simply as herpes, is a viral infection caused by the herpes simplex virus. Herpes infections are categorized by the area of the body that is infected. The two major types of herpes are oral herpes and genital herpes, though other forms also exist.

Neonatal herpes simplex, or simply neonatal herpes, is a herpes infection in a newborn baby, caused by the herpes simplex virus (HSV). It occurs mostly as a result of vertical transmission of the HSV from an affected mother to her baby. Types include skin, eye, and mouth herpes (SEM), disseminated herpes (DIS), and central nervous system herpes (CNS). Depending on the type, symptoms vary from a fever to small blisters, irritability, low body temperature, lethargy, breathing difficulty, and a large abdomen due to ascites or large liver. There may be red streaming eyes or no symptoms.
Herpes meningitis is inflammation of the meninges, the protective tissues surrounding the spinal cord and brain, due to infection from viruses of the Herpesviridae family - the most common amongst adults is HSV-2. Symptoms are self-limiting over 2 weeks with severe headache, nausea, vomiting, neck-stiffness, and photophobia. Herpes meningitis can cause Mollaret's meningitis, a form of recurrent meningitis. Lumbar puncture with cerebrospinal fluid results demonstrating aseptic meningitis pattern is necessary for diagnosis and polymerase chain reaction is used to detect viral presence. Although symptoms are self-limiting, treatment with antiviral medication may be recommended to prevent progression to Herpes Meningoencephalitis.

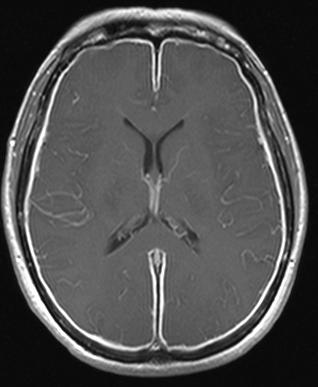
Herpes simplex encephalitis (HSE), or simply herpes encephalitis, is encephalitis due to herpes simplex virus. It is estimated to affect at least 1 in 500,000 individuals per year, and some studies suggest an incidence rate of 5.9 cases per 100,000 live births.
Neurovirology is an interdisciplinary field which represents a melding of clinical neuroscience, virology, immunology, and molecular biology. The main focus of the field is to study viruses capable of infecting the nervous system. In addition to this, the field studies the use of viruses to trace neuroanatomical pathways, for gene therapy, and to eliminate detrimental populations of neural cells.

Neonatal meningitis is a serious medical condition in infants that is rapidly fatal if untreated. Meningitis, an inflammation of the meninges, the protective membranes of the central nervous system, is more common in the neonatal period than any other time in life, and is an important cause of morbidity and mortality globally. Mortality is roughly half in developing countries and ranges from 8%-12.5% in developed countries.
Jamestown Canyon encephalitis is an infectious disease caused by the Jamestown Canyon virus, an orthobunyavirus of the California serogroup. It is mainly spread during the summer by different mosquito species in the United States and Canada.










