Otorhinolaryngology is a surgical subspecialty within medicine that deals with the surgical and medical management of conditions of the head and neck. Doctors who specialize in this area are called otorhinolaryngologists, otolaryngologists, head and neck surgeons, or ENT surgeons or physicians.

The parotid gland is a major salivary gland in many animals. In humans, the two parotid glands are present on either side of the mouth and in front of both ears. They are the largest of the salivary glands. Each parotid is wrapped around the mandibular ramus, and secretes serous saliva through the parotid duct into the mouth, to facilitate mastication and swallowing and to begin the digestion of starches. There are also two other types of salivary glands; they are submandibular and sublingual glands. Sometimes accessory parotid glands are found close to the main parotid glands.

An adenoma is a benign tumor of epithelial tissue with glandular origin, glandular characteristics, or both. Adenomas can grow from many glandular organs, including the adrenal glands, pituitary gland, thyroid, prostate, and others. Some adenomas grow from epithelial tissue in nonglandular areas but express glandular tissue structure. Although adenomas are benign, they should be treated as pre-cancerous. Over time adenomas may transform to become malignant, at which point they are called adenocarcinomas. Most adenomas do not transform. However, even though benign, they have the potential to cause serious health complications by compressing other structures and by producing large amounts of hormones in an unregulated, non-feedback-dependent manner. Some adenomas are too small to be seen macroscopically but can still cause clinical symptoms.

The paired submandibular glands are major salivary glands located beneath the floor of the mouth. In adult humans, they each weigh about 15 grams and contribute some 60–67% of unstimulated saliva secretion; on stimulation their contribution decreases in proportion as parotid gland secretion rises to 50%. The average length of the normal adult human submandibular salivary gland is approximately 27 mm, while the average width is approximately 14.3 mm.

Adenoid cystic carcinoma is a rare type of cancer that can exist in many different body sites. This tumor most often occurs in the salivary glands, but it can also be found in many anatomic sites, including the breast, lacrimal gland, lung, brain, Bartholin gland, trachea, and the paranasal sinuses.

A facelift, technically known as a rhytidectomy, is a type of cosmetic surgery procedure intended to give a more youthful facial appearance. There are multiple surgical techniques and exercise routines. Surgery usually involves the removal of excess facial skin, with or without the tightening of underlying tissues, and the redraping of the skin on the patient's face and neck. Exercise routines tone underlying facial muscles without surgery. Surgical facelifts are effectively combined with eyelid surgery (blepharoplasty) and other facial procedures and are typically performed under general anesthesia or deep twilight sleep.
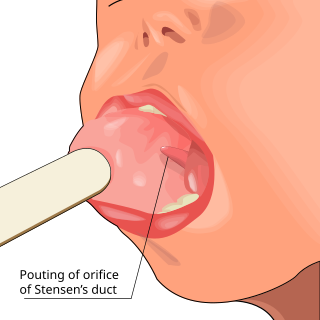
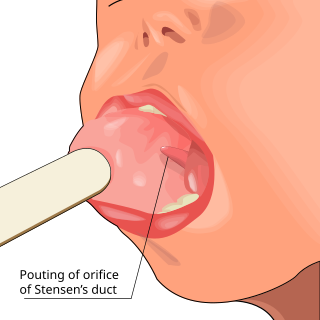
Parotitis is an inflammation of one or both parotid glands, the major salivary glands located on either side of the face, in humans. The parotid gland is the salivary gland most commonly affected by inflammation.
An oncocytoma is a tumor made up of oncocytes, epithelial cells characterized by an excessive amount of mitochondria, resulting in an abundant acidophilic, granular cytoplasm. The cells and the tumor that they compose are often benign but sometimes may be premalignant or malignant.

Warthin's tumor, also known as papillary cystadenoma lymphomatosum, is a benign cystic tumor of the salivary glands containing abundant lymphocytes and germinal centers. It is named for pathologist Aldred Scott Warthin, who described two cases in 1929.

Pleomorphic adenoma is a common benign salivary gland neoplasm characterised by neoplastic proliferation of epithelial (ductal) cells along with myoepithelial components, having a malignant potentiality. It is the most common type of salivary gland tumor and the most common tumor of the parotid gland. It derives its name from the architectural Pleomorphism seen by light microscopy. It is also known as "Mixed tumor, salivary gland type", which refers to its dual origin from epithelial and myoepithelial elements as opposed to its pleomorphic appearance.
Hepatectomy is the surgical resection of the liver. While the term is often employed for the removal of the liver from a liver transplant donor, this article will focus on partial resections of hepatic tissue and hepatoportoenterostomy.

Canalicular adenoma is a type of growth that occurs in human salivary glands. It is a benign growth which occurs in the epithelial cells, and is typically arranged in columns of cells that form interconnecting cords. Canalicular adenoma is a very rare benign neoplasm; it constitutes about 1% of all salivary gland tumors and about 4% of all benign salivary gland tumors.

The marginal mandibular branch of the facial nerve arises from the facial nerve in the parotid gland at the parotid plexus. It passes anterior-ward deep to the platysma and depressor anguli oris muscles. It provides motor innervation to muscles of the lower lip and chin: the depressor labii inferioris muscle, depressor anguli oris muscle, and mentalis muscle. It communicates with the mental branch of the inferior alveolar nerve.

Frey's syndrome is a rare neurological disorder resulting from damage to or near the parotid glands responsible for making saliva, and from damage to the auriculotemporal nerve often from surgery.

Acinic cell carcinoma is a malignant tumor representing 2% of all salivary tumors. 90% of the time found in the parotid gland, 10% intraorally on buccal mucosa or palate. The disease presents as a slow growing mass, associated with pain or tenderness in 50% of the cases. Often appears pseudoencapsulated.

Salivary gland tumours, or neoplasms, are tumours that form in the tissues of salivary glands. The salivary glands are classified as major or minor. The major salivary glands consist of the parotid, submandibular, and sublingual glands. The minor salivary glands consist of 800 to 1000 small mucus-secreting glands located throughout the lining of the oral cavity. People with these types of tumours may be asymptomatic.

Myoepithelioma of the head and neck, also myoepithelioma, is a salivary gland tumour of the head and neck that is usually benign. When malignant, which is exceedingly rare, they are known as malignant myoepithelioma or Myoepithelial carcinoma, and they account for 1% of the salivary tumors with poor prognosis.

Epithelial-myoepithelial carcinoma (EMCa) is a rare malignant tumour that typically arises in a salivary gland and consists of both an epithelial and myoepithelial component. They are predominantly found in the parotid gland and represent approximately 1% of salivary gland tumours.

Ceruminous adenocarcinoma is a malignant neoplasm derived from ceruminous glands of the external auditory canal. This tumor is rare, with several names used in the past. Synonyms have included cylindroma, ceruminoma, ceruminous adenocarcinoma, not otherwise specified (NOS), ceruminous adenoid cystic carcinoma (ACC), and ceruminous mucoepidermoid carcinoma.

Carcinoma ex pleomorphic adenoma is a type of cancer typically found in the parotid gland. It arises from the benign tumour pleomorphic adenoma.