Related Research Articles

In humans and other primates, the knee joins the thigh with the leg and consists of two joints: one between the femur and tibia, and one between the femur and patella. It is the largest joint in the human body. The knee is a modified hinge joint, which permits flexion and extension as well as slight internal and external rotation. The knee is vulnerable to injury and to the development of osteoarthritis.

In human anatomy, a hamstring is any one of the three posterior thigh muscles between the hip and the knee.

The tibia, also known as the shinbone or shankbone, is the larger, stronger, and anterior (frontal) of the two bones in the leg below the knee in vertebrates ; it connects the knee with the ankle. The tibia is found on the medial side of the leg next to the fibula and closer to the median plane. The tibia is connected to the fibula by the interosseous membrane of leg, forming a type of fibrous joint called a syndesmosis with very little movement. The tibia is named for the flute tibia. It is the second largest bone in the human body, after the femur. The leg bones are the strongest long bones as they support the rest of the body.
The ankle, the talocrural region or the jumping bone (informal) is the area where the foot and the leg meet. The ankle includes three joints: the ankle joint proper or talocrural joint, the subtalar joint, and the inferior tibiofibular joint. The movements produced at this joint are dorsiflexion and plantarflexion of the foot. In common usage, the term ankle refers exclusively to the ankle region. In medical terminology, "ankle" can refer broadly to the region or specifically to the talocrural joint.

The anterior cruciate ligament (ACL) is one of a pair of cruciate ligaments in the human knee. The two ligaments are also called "cruciform" ligaments, as they are arranged in a crossed formation. In the quadruped stifle joint, based on its anatomical position, it is also referred to as the cranial cruciate ligament. The term cruciate translates to cross. This name is fitting because the ACL crosses the posterior cruciate ligament to form an "X". It is composed of strong, fibrous material and assists in controlling excessive motion. This is done by limiting mobility of the joint. The anterior cruciate ligament is one of the four main ligaments of the knee, providing 85% of the restraining force to anterior tibial displacement at 30 and 90° of knee flexion. The ACL is the most injured ligament of the four located in the knee.

The tibialis posterior muscle is the most central of all the leg muscles, and is located in the deep posterior compartment of the leg. It is the key stabilizing muscle of the lower leg.

The flexor digitorum longus muscle is situated on the tibial side of the leg. At its origin it is thin and pointed, but it gradually increases in size as it descends. It serves to flex the second, third, fourth, and fifth toes.

The plantaris is one of the superficial muscles of the superficial posterior compartment of the leg, one of the fascial compartments of the leg.
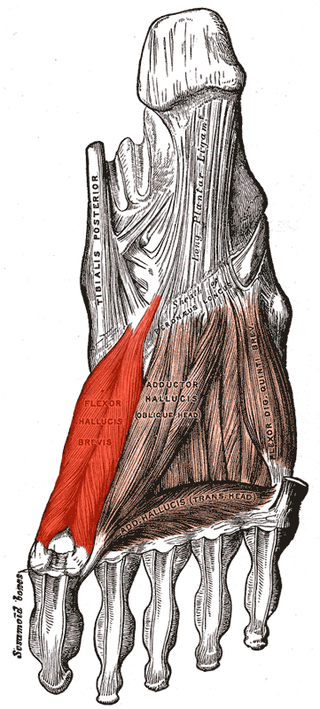
Flexor hallucis brevis muscle is a muscle of the foot that flexes the big toe.

An ankle fracture is a break of one or more of the bones that make up the ankle joint. Symptoms may include pain, swelling, bruising, and an inability to walk on the injured leg. Complications may include an associated high ankle sprain, compartment syndrome, stiffness, malunion, and post-traumatic arthritis.
The knee examination, in medicine and physiotherapy, is performed as part of a physical examination, or when a patient presents with knee pain or a history that suggests a pathology of the knee joint.
The flexor retinaculum of foot is a strong fibrous band in the foot.

The unhappy triad, also known as a blown knee among other names, is an injury to the anterior cruciate ligament, medial collateral ligament, and meniscus. Analysis during the 1990s indicated that this 'classic' O'Donoghue triad is actually an unusual clinical entity among athletes with knee injuries. Some authors mistakenly believe that in this type of injury, "combined anterior cruciate and medial collateral ligament disruptions that were incurred during athletic endeavors" always present with concomitant medial meniscus injury. However, the 1990 analysis showed that lateral meniscus tears are more common than medial meniscus tears in conjunction with sprains of the ACL.

A malleolus is the bony prominence on each side of the human ankle.
Foot and ankle surgery is a sub-specialty of orthopedics and podiatry that deals with the treatment, diagnosis and prevention of disorders of the foot and ankle. Orthopaedic surgeons are medically qualified, having been through four years of college, followed by 4 years of medical school or osteopathic medical school to obtain an M.D. or D.O. followed by specialist training as a resident in orthopaedics, and only then do they sub-specialise in foot and ankle surgery. Training for a podiatric foot and ankle surgeon consists of four years of college, four years of podiatric medical school (D.P.M.), 3–4 years of a surgical residency and an optional 1 year fellowship.

Pes anserine bursitis is an inflammatory condition of the medial (inner) knee at the anserine bursa, a sub muscular bursa, just below the pes anserinus.
Posterolateral corner injuries of the knee are injuries to a complex area formed by the interaction of multiple structures. Injuries to the posterolateral corner can be debilitating to the person and require recognition and treatment to avoid long term consequences. Injuries to the PLC often occur in combination with other ligamentous injuries to the knee; most commonly the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL). As with any injury, an understanding of the anatomy and functional interactions of the posterolateral corner is important to diagnosing and treating the injury.

Ulnar collateral ligament injuries can occur during certain activities such as overhead baseball pitching. Acute or chronic disruption of the ulnar collateral ligament result in medial elbow pain, valgus instability, and impaired throwing performance. There are both non-surgical and surgical treatment options.

Medial knee injuries are the most common type of knee injury. The medial ligament complex of the knee consists of:

Sinus tarsi syndrome is the clinical disorder of pain and tenderness in the sinus tarsi, which is a lateral tunnel in the foot at the junction of the hindfoot and the midfoot, between the ankle and the heel. Most of the time, sinus tarsi syndrome onsets after ankle sprains, however there can be other causes. There are a variety of treatments, divided into conservative treatments such as physical and orthotic therapy, and more invasive ones such as cortisone injections. The condition is somewhat poorly understood and is subject to heavy debate in the medical community.
References
- 1 2 3 4 5 6 7 8 "Posterior Tibial Tendon Dysfunction (PTTD): Symptoms & Treatment". Cleveland Clinic. Retrieved 2022-12-23.
- 1 2 3 4 5 6 7 8 9 10 11 Knapp, Paul W.; Constant, Dustin (2022), "Posterior Tibial Tendon Dysfunction", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 31194317 , retrieved 2022-12-23
- 1 2 "Posterior Tibial Tendon Dysfunction (PTTD) - Foot Health Facts". www.foothealthfacts.org. Retrieved 2022-12-23.
- ↑ "Posterior Tibial Tendon Dysfunction - OrthoInfo - AAOS". www.orthoinfo.org. Retrieved 2022-12-23.