| Neuromuscular disease | |
|---|---|
 | |
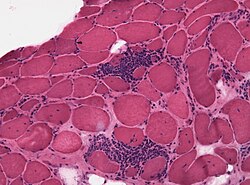
| Congenital nemaline myopathy (neuromuscular disorder) | |
| Specialty | Neurology, neuromuscular medicine, physical medicine and rehabilitation |
| Causes | Autoimmune disorders, [1] genetic disorders, [2] environmental factors [3] |
| Diagnostic method | Muscle electrophysiology tests, genetic testing |
| Treatment | Depends on the disorder; many currently have no cure [2] |
A neuromuscular disease is any disease affecting the peripheral nervous system (PNS), [a] the neuromuscular junctions, or skeletal muscles, all of which are components of the motor unit. [4] Damage to any of these structures can cause muscle atrophy and weakness. Issues with sensation can also occur.
Contents
- Signs and symptoms
- Causes
- Diagnosis
- Prognosis
- See also
- Notes
- References
- Further reading
- External links
Neuromuscular diseases can be acquired or genetic. Mutations of more than 650 genes have shown to be causes of neuromuscular diseases. [5] [6] [7] Other causes include nerve or muscle degeneration, autoimmunity, toxins, medications, malnutrition, metabolic derangements, hormone imbalances, infection, nerve compression/entrapment, comprised blood supply, and trauma. [8]