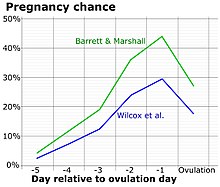
Fertility awareness (FA) refers to a set of practices used to determine the fertile and infertile phases of a woman's menstrual cycle. Fertility awareness methods may be used to avoid pregnancy, to achieve pregnancy, or as a way to monitor gynecological health.

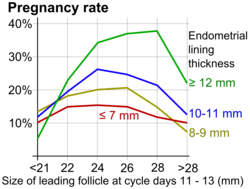
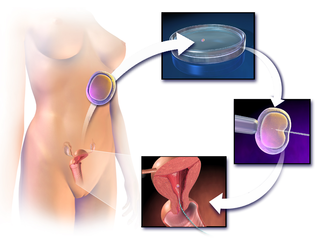
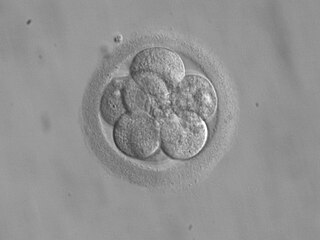
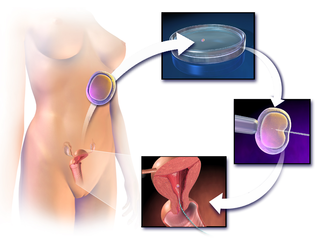
In vitro fertilisation (IVF) is a process of fertilisation in which an egg is combined with sperm in vitro. The process involves monitoring and stimulating a woman's ovulatory process, then removing an ovum or ova from her ovaries and enabling a man's sperm to fertilise them in a culture medium in a laboratory. After a fertilised egg (zygote) undergoes embryo culture for 2–6 days, it is transferred by catheter into the uterus, with the intention of establishing a successful pregnancy.

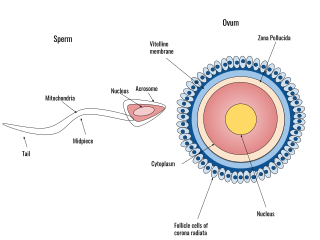
Intracytoplasmic sperm injection is an in vitro fertilization (IVF) procedure in which a single sperm cell is injected directly into the cytoplasm of an egg. This technique is used in order to prepare the gametes for the obtention of embryos that may be transferred to a maternal uterus. With this method, the acrosome reaction is skipped.

Ovulation is an important part of the menstrual cycle in female vertebrates where the egg cells are released from the ovaries as part of the ovarian cycle. In female humans ovulation typically occurs near the midpoint in the menstrual cycle and after the follicular phase. Ovulation is stimulated by an increase in luteinizing hormone (LH). The ovarian follicles rupture and release the secondary oocyte ovarian cells.

Artificial insemination is the deliberate introduction of sperm into a female's cervix or uterine cavity for the purpose of achieving a pregnancy through in vivo fertilization by means other than sexual intercourse. It is a fertility treatment for humans, and is a common practice in animal breeding, including dairy cattle and pigs.
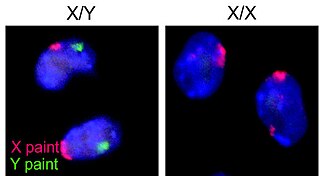
Assisted reproductive technology (ART) includes medical procedures used primarily to address infertility. This subject involves procedures such as in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), cryopreservation of gametes or embryos, and/or the use of fertility medication. When used to address infertility, ART may also be referred to as fertility treatment. ART mainly belongs to the field of reproductive endocrinology and infertility. Some forms of ART may be used with regard to fertile couples for genetic purpose. ART may also be used in surrogacy arrangements, although not all surrogacy arrangements involve ART. The existence of sterility will not always require ART to be the first option to consider, as there are occasions when its cause is a mild disorder that can be solved with more conventional treatments or with behaviors based on promoting health and reproductive habits.
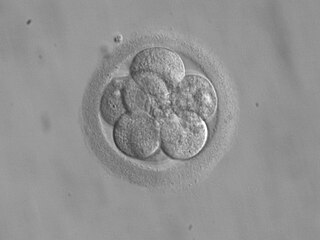
Embryo transfer refers to a step in the process of assisted reproduction in which embryos are placed into the uterus of a female with the intent to establish a pregnancy. This technique - which is often used in connection with in vitro fertilization (IVF) - may be used in humans or in other animals, in which situations and goals may vary.
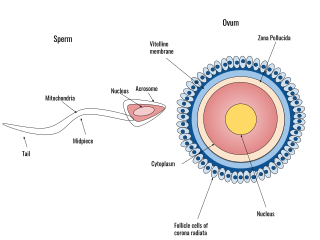
Human fertilization is the union of an egg and sperm, occurring primarily in the ampulla of the fallopian tube. The result of this union leads to the production of a fertilized egg called a zygote, initiating embryonic development. Scientists discovered the dynamics of human fertilization in the 19th century.
Human sexual reproduction, to produce offspring, begins with fertilization. Successful reproduction typically involves sexual intercourse between a healthy, sexually mature and fertile male and female. Because of ejaculation during intercourse, the male reproductive system deposits semen containing sperm into the female reproductive system, which can result in the fertilization of an ovum, to form a zygote.
Ovulation induction is the stimulation of ovulation by medication. It is usually used in the sense of stimulation of the development of ovarian follicles to reverse anovulation or oligoovulation.

Fertility clinics are medical clinics that assist couples, and sometimes individuals, who want to become parents but for medical reasons have been unable to achieve this goal via the natural course. Clinics apply a number of diagnosis tests and sometimes very advanced medical treatments to achieve conceptions and pregnancies.

In vitro maturation (IVM) is the technique of letting the contents of ovarian follicles and the oocytes inside mature in vitro. It can be offered to women with infertility problems, combined with In Vitro Fertilization (IVF), offering women pregnancy without ovarian stimulation.
Poor ovarian reserve is a condition of low fertility characterized by 1): low numbers of remaining oocytes in the ovaries or 2) possibly impaired preantral oocyte development or recruitment. Recent research suggests that premature ovarian aging and premature ovarian failure may represent a continuum of premature ovarian senescence. It is usually accompanied by high FSH levels.
Unexplained infertility is infertility that is idiopathic in the sense that its cause remains unknown even after an infertility work-up, usually including semen analysis in the man and assessment of ovulation and fallopian tubes in the woman. It is usually an exercise in excluding all possible causes before making a diagnosis, however the age of the female partner as well as the duration of infertility are often the most scrutinized characteristics of any infertility case.

Fertility testing is the process by which fertility is assessed, both generally and also to find the "fertile window" in the menstrual cycle. General health affects fertility, and STI testing is an important related field.
Infertility in polycystic ovary disease (PCOS) is a hormonal imbalance in women that is thought to be one of the leading causes of female infertility. Polycystic ovary syndrome causes more than 75% of cases of anovulatory infertility.
Partner-assisted reproduction, reception of oocytes from partner (ROPA), reciprocal IVF,shared motherhood, partner IVF or co-IVF is a method of family building that is used by couples who both possess female reproductive organs. The method uses in vitro fertilization (IVF), a method that means eggs are removed from the ovaries, fertilized in a laboratory, and then one or more of the resulting embryos are placed in the uterus to hopefully create a pregnancy. Reciprocal IVF differs from standard IVF in that two partners are involved: the eggs are taken from one partner, and the other partner carries the pregnancy. In this way, the process is mechanically identical to IVF with egg donation. Reciprocal IVF offers the highest chance for pregnancy and a lower chance of a multiple births.
Induction of final maturation of oocytes is a procedure that is usually performed as part of controlled ovarian hyperstimulation to render the oocytes fully developed and thereby resulting in optimal pregnancy chances. It is basically a replacement for the luteinizing hormone (LH) surge whose effects include final maturation in natural menstrual cycles.
Antisperm antibodies (ASA) are antibodies produced against sperm antigens.

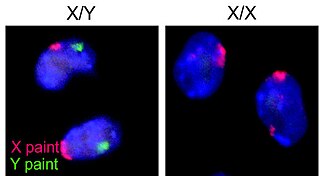
Lesbian, gay, bisexual, and transgender people people wishing to have children may use assisted reproductive technology. In recent decades, developmental biologists have been researching and developing techniques to facilitate same-sex reproduction.