Regimen alternatives

The main alternatives for ovulation induction medications are:
- Antiestrogen, causing an inhibition of the negative feedback of estrogen on the pituitary gland, resulting in an increase in secretion of follicle-stimulating hormone. Medications in use for this effect are mainly clomifene citrate and tamoxifen (both being selective estrogen-receptor modulators), as well as letrozole (an aromatase inhibitor).[ citation needed ]
- Follicle-stimulating hormone, directly stimulating the ovaries. In women with anovulation, it may be an alternative after 7 to 12 attempted cycles of antiestrogens (as evidenced by clomifene citrate), since the latter ones are less expensive and more easy to control. [9]
Antiestrogens
Clomifene citrate
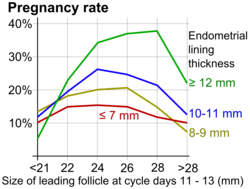
Clomifene citrate (Clomid is a common brand name) is the medication which is most commonly used to treat anovulation. It is a selective estrogen-receptor modulator, affecting the hypothalamic–pituitary–gonadal axis to respond as if there was an estrogen deficit in the body, in effect increasing the production of follicle-stimulating hormone. It is relatively easy and convenient to use. [10] Clomifene appears to inhibit estrogen receptors in hypothalamus, thereby inhibiting negative feedback of estrogen on production of follicle-stimulating hormone. [11] It may also result in direct stimulation of the hypothalamic–pituitary axis. [11] It also has an effect on cervical mucus quality and uterine mucosa, which might affect sperm penetration and survival, hence its early administration during the menstrual cycle. Clomifene citrate is a very efficient ovulation inductor, and has a success rate of 67%. Nevertheless, it only has a 37% success rate in inducing pregnancy. This difference may be due to the anti-estrogenic effect which clomifene citrate has on the endometrium, cervical mucus, uterine blood flow, as well as the resulting decrease in the motility of the fallopian tubes and the maturation of the oocytes. [12]
Letrozole
Letrozole has been used for ovarian stimulation by fertility doctors since 2001 because it has fewer side-effects than clomiphene and less chance of multiple gestation.[ citation needed ] A study of 150 babies following treatment with letrozole or letrozole and follicle-stimulating hormone presented at the American Society of Reproductive Medicine 2005 Conference found no difference in overall abnormalities but did find a significantly higher rate of locomotor and cardiac abnormalities among the group having taken letrozole compared to natural conception. [13] A larger, follow-up study with 911 babies compared those born following treatment with letrozole to those born following treatment with clomiphene. [14] That study also found no significant difference in the rate of overall abnormalities, but found that congenital cardiac anomalies was significantly higher in the clomiphene group compared to the letrozole group.
Dosage is generally 2.5 to 7.5 mg daily over 5 days. A higher dose of up to 12.5 mg per day results in increased follicular growth and a higher number of predicted ovulations, without a detrimental effect on endometrial thickness, and is considered in those who do not respond adequately to a lower dose. [15]
Tamoxifen
Tamoxifen affects estrogen receptors in a similar fashion as clomifene citrate. It is often used in the prevention and treatment of breast cancer. It can therefore also be used to treat patients that have a reaction to clomifene citrate. [16]
Follicle-stimulating hormone
Preparations of follicle-stimulating hormone mainly include those derived from the urine of menopausal women, as well as recombinant preparations. The recombinant preparations are more pure and more easily administered, but they are more expensive. The urinary preparations are equally effective and less expensive, but are not as convenient to administer as they are available in vials versus injection pens.
Gonadotropin-releasing hormone pump
The gonadotropin-releasing hormone pump is used to release doses in a pulsatile fashion. This hormone is synthesised by the hypothalamus and induces the secretion of follicle-stimulating hormone by the pituitary gland. Gonadotropin-releasing hormone must be delivered in a pulsatile fashion to imitate the random secretion of the hypothalamus in order to stimulate the pituitary into secreting luteinizing hormone and follicle-stimulating hormone. The gonadotropin-releasing hormone pump is the size of a cigarette box and has a small catheter. Unlike other treatments, using the gonadotropin-releasing hormone pump usually does not result in multiple pregnancies. Filicori from the University of Bologna suggests that this might be because gonadotrophins are absent when the treatment is initiated, and therefore the hormones released by the pituitary (luteinizing hormone and follicle-stimulating hormone) can still take part in the retro-control of gonadotrophin secretion, mimicking the natural cycle. [17] This treatment can also be used for underweight and/or anorexic patients; [18] it has also been used in certain cases of hyperprolactinemia.
National and regional usage
In the Nordic countries, letrozole is practically the standard initial regimen used for ovulation induction, since no formulation of clomifene is registered for use there. [19] [20]
India banned the usage of letrozole in 2011, citing potential risks to infants. [21] In 2012, an Indian parliamentary committee said that the drug controller office colluded with letrozole's makers to approve the drug for infertility in India. [22]