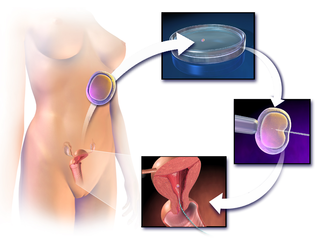
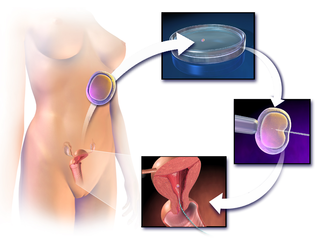
In vitro fertilisation (IVF) is a process of fertilisation where an egg is combined with sperm in vitro. The process involves monitoring and stimulating a woman's ovulatory process, removing an ovum or ova from their ovaries and letting a man's sperm fertilise them in a culture medium in a laboratory. After the fertilised egg (zygote) undergoes embryo culture for 2–6 days, it is transferred by catheter into the uterus, with the intention of establishing a successful pregnancy.

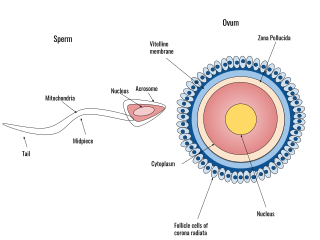
Intracytoplasmic sperm injection is an in vitro fertilization (IVF) procedure in which a single sperm cell is injected directly into the cytoplasm of an egg. This technique is used in order to prepare the gametes for the obtention of embryos that may be transferred to a maternal uterus. With this method, the acrosome reaction is skipped.

For fertilization to happen between a sperm and egg cell, a sperm must first fuse with the plasma membrane and then penetrate the female egg cell to fertilize it. While the fusion of the sperm cell with the egg cell's plasma membrane is relatively straightforward, penetrating the egg's protective layers, such as the zona pellucida, presents a significant challenge. Therefore, sperm cells go through a process known as the acrosome reaction, which is the reaction that occurs in the acrosome of the sperm as it approaches the egg.

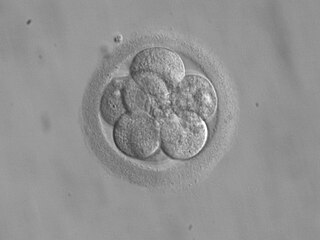
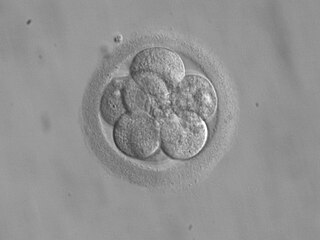
Preimplantation genetic diagnosis is the genetic profiling of embryos prior to implantation, and sometimes even of oocytes prior to fertilization. PGD is considered in a similar fashion to prenatal diagnosis. When used to screen for a specific genetic disease, its main advantage is that it avoids selective abortion, as the method makes it highly likely that the baby will be free of the disease under consideration. PGD thus is an adjunct to assisted reproductive technology, and requires in vitro fertilization (IVF) to obtain oocytes or embryos for evaluation. Embryos are generally obtained through blastomere or blastocyst biopsy. The latter technique has proved to be less deleterious for the embryo, therefore it is advisable to perform the biopsy around day 5 or 6 of development.

Oogenesis, ovogenesis, or oögenesis is the differentiation of the ovum into a cell competent to further develop when fertilized. It is developed from the primary oocyte by maturation. Oogenesis is initiated in the embryonic stage.
Assisted reproductive technology (ART) includes medical procedures used primarily to address infertility. This subject involves procedures such as in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), cryopreservation of gametes or embryos, and/or the use of fertility medication. When used to address infertility, ART may also be referred to as fertility treatment. ART mainly belongs to the field of reproductive endocrinology and infertility. Some forms of ART may be used with regard to fertile couples for genetic purpose. ART may also be used in surrogacy arrangements, although not all surrogacy arrangements involve ART. The existence of sterility will not always require ART to be the first option to consider, as there are occasions when its cause is a mild disorder that can be solved with more conventional treatments or with behaviors based on promoting health and reproductive habits.
Embryo transfer refers to a step in the process of assisted reproduction in which embryos are placed into the uterus of a female with the intent to establish a pregnancy. This technique - which is often used in connection with in vitro fertilization (IVF) - may be used in humans or in other animals, in which situations and goals may vary.
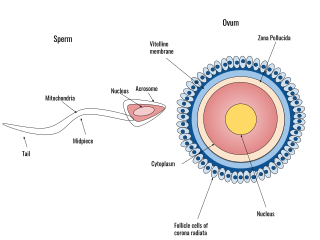
Human fertilization is the union of an egg and sperm, occurring primarily in the ampulla of the fallopian tube. The result of this union leads to the production of a fertilized egg called a zygote, initiating embryonic development. Scientists discovered the dynamics of human fertilization in the 19th century.
The hamster zona-free ovum test, or hamster egg-penetration test, or sometimes just hamster test, is an in-vitro test used to study physiological profile of spermatozoa. The primary application of the test is to diagnose male infertility caused by sperm unable to penetrate the ova. The test has limited value, due to expense and a high false negative rate.

Oocyte cryopreservation is a procedure to preserve a woman's eggs (oocytes). This technique has been used to postpone pregnancy. When pregnancy is desired, the eggs can be thawed, fertilized, and transferred to the uterus as embryos. Several studies have shown that most infertility problems are due to germ cell deterioration related to aging. The procedure's success rate varies depending on the age of the woman,, as well as depending on health and genetic indicators. In 1986, the first human birth of oocyte oocyte cryopreservation was reported.
Controlled ovarian hyperstimulation is a technique used in assisted reproduction involving the use of fertility medications to induce ovulation by multiple ovarian follicles. These multiple follicles can be taken out by oocyte retrieval for use in in vitro fertilisation (IVF), or be given time to ovulate, resulting in superovulation which is the ovulation of a larger-than-normal number of eggs, generally in the sense of at least two. When ovulated follicles are fertilised in vivo, whether by natural or artificial insemination, there is a very high risk of a multiple pregnancy.

In vitro maturation (IVM) is the technique of letting the contents of ovarian follicles and the oocytes inside mature in vitro. It can be offered to women with infertility problems, combined with In Vitro Fertilization (IVF), offering women pregnancy without ovarian stimulation.
Poor ovarian reserve is a condition of low fertility characterized by 1): low numbers of remaining oocytes in the ovaries or 2) possibly impaired preantral oocyte development or recruitment. Recent research suggests that premature ovarian aging and premature ovarian failure may represent a continuum of premature ovarian senescence. It is usually accompanied by high FSH levels.
Transvaginal oocyte retrieval (TVOR), also referred to as oocyte retrieval (OCR), is a technique used in in vitro fertilization (IVF) in order to remove oocytes from an ovary, enabling fertilization outside the body. Transvaginal oocyte retrieval is more properly referred to as transvaginal ovum retrieval when the oocytes have matured into ova, as is normally the case in IVF. It can be also performed for egg donation, oocyte cryopreservation and other assisted reproduction technology such as ICSI.
Fertility preservation is the effort to help cancer patients retain their fertility, or ability to procreate. Research into how cancer, ageing and other health conditions effect reproductive health and preservation options are growing. Specifically sparked in part by the increase in the survival rate of cancer patients.
Embryo quality is the ability of an embryo to perform successfully in terms of conferring a high pregnancy rate and/or resulting in a healthy person. Embryo profiling is the estimation of embryo quality by qualification and/or quantification of various parameters. Estimations of embryo quality guides the choice in embryo selection in in vitro fertilization.
Polar body biopsy is the sampling of a polar body of an oocyte. It was first applied clinically in humans in 1987 after extensive animal studies. A polar body is a small haploid cell that is formed concomitantly as an egg cell during oogenesis, but which generally does not have the ability to be fertilized.
Morphokinetics (‘morpho’’ form/shape and ‘kinetics’ movement) refers to time specific morphological changes during embryo development providing dynamic information on a fertilized egg. The detailed information eases morphological selection of embryos with high implantation potential to be used in In-Vitro Fertilisation treatment.
Repeated implantation failure (RIF) is the repeated failure of the embryo to implant onto the side of the uterus wall following IVF treatment. Implantation happens at 6–7 days after conception and involves the embedding of the growing embryo into the mothers uterus and a connection being formed. A successful implantation can be determined by using an ultrasound to view the sac which the baby grows in, inside the uterus.
Dmitri Dozortsev is a Russian-American physician scientist, inventor and researcher. Dozortsev's contributions in research and publications are mostly in the areas of human reproductive medicine and biology. In particular, he is best known for his studies of in vitro fertilisation and embryo transfer. Dozortsev currently serves as President of the American College of Embryology and as Director of Omni-Med laboratories.