Myoclonic epilepsy refers to a family of epilepsies that present with myoclonus. It starts in both sides of the body at once, and last for more than a second or two. When myoclonic jerks are occasionally associated with abnormal brain wave activity, it can be categorized as myoclonic seizure. If the abnormal brain wave activity is persistent and results from ongoing seizures, then a diagnosis of myoclonic epilepsy may be considered. Myoclonic seizures frequently occur in day-to-day life. During sleep, abrupt jerks and hiccups occurred.
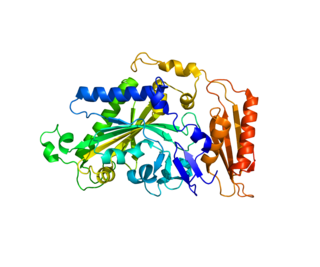
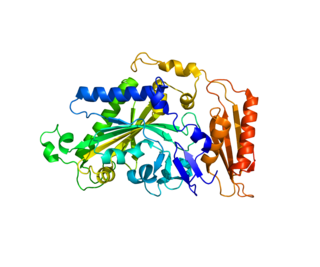
Glucose transporter 1, also known as solute carrier family 2, facilitated glucose transporter member 1 (SLC2A1), is a uniporter protein that in humans is encoded by the SLC2A1 gene. GLUT1 facilitates the transport of glucose across the plasma membranes of mammalian cells. This gene encodes a facilitative glucose transporter that is highly expressed in erythrocytes and endothelial cells, including cells of the blood–brain barrier. The encoded protein is found primarily in the cell membrane and on the cell surface, where it can also function as a receptor for human T-cell leukemia virus (HTLV) I and II. GLUT1 accounts for 2 percent of the protein in the plasma membrane of erythrocytes. Mutations in this gene can cause GLUT1 deficiency syndrome 1, GLUT1 deficiency syndrome 2, idiopathic generalized epilepsy 12, dystonia 9, and stomatin-deficient cryohydrocytosis.

Aminomethyltransferase is an enzyme that catabolizes the creation of methylenetetrahydrofolate. It is part of the glycine decarboxylase complex.
Progressive Myoclonic Epilepsies (PME) are a rare group of inherited neurodegenerative diseases characterized by myoclonus, resistance to treatment, and neurological deterioration. The cause of PME depends largely on the type of PME. Most PMEs are caused by autosomal dominant or recessive and mitochondrial mutations. The location of the mutation also affects the inheritance and treatment of PME. Diagnosing PME is difficult due to their genetic heterogeneity and the lack of a genetic mutation identified in some patients. The prognosis depends largely on the worsening symptoms and failure to respond to treatment. There is no current cure for PME and treatment focuses on managing myoclonus and seizures through antiepileptic medication (AED).
Ohtahara syndrome (OS), also known as early infantile epileptic encephalopathy (EIEE) is a progressive epileptic encephalopathy. The syndrome is outwardly characterized by tonic spasms and partial seizures within the first few months of life, and receives its more elaborate name from the pattern of burst activity on an electroencephalogram (EEG). It is an extremely debilitating progressive neurological disorder, involving intractable seizures and severe intellectual disabilities. No single cause has been identified, although in many cases structural brain damage is present.

Sodium channel protein type 1 subunit alpha (SCN1A), is a protein which in humans is encoded by the SCN1A gene.

Phosphate carrier protein, mitochondrial is a protein that in humans is encoded by the SLC25A3 gene. The encoded protein is a transmembrane protein located in the mitochondrial inner membrane and catalyzes the transport of phosphate ions across it for the purpose of oxidative phosphorylation. There are two significant isoforms of this gene expressed in human cells, which differ slightly in structure and function. Mutations in this gene can cause mitochondrial phosphate carrier deficiency (MPCD), a fatal disorder of oxidative phosphorylation symptomized by lactic acidosis, neonatal hypotonia, hypertrophic cardiomyopathy, and death within the first year of life.

The mitochondrial dicarboxylate carrier (DIC) is an integral membrane protein encoded by the SLC25A10 gene in humans that catalyzes the transport of dicarboxylates such as malonate, malate, and succinate across the inner mitochondrial membrane in exchange for phosphate, sulfate, and thiosulfate by a simultaneous antiport mechanism, thus supplying substrates for the Krebs cycle, gluconeogenesis, urea synthesis, fatty acid synthesis, and sulfur metabolism.

FAD-dependent oxidoreductase domain-containing protein 1 (FOXRED1), also known as H17, or FP634 is an enzyme that in humans is encoded by the FOXRED1 gene. FOXRED1 is an oxidoreductase and complex I-specific molecular chaperone involved in the assembly and stabilization of NADH dehydrogenase (ubiquinone) also known as complex I, which is located in the mitochondrial inner membrane and is the largest of the five complexes of the electron transport chain. Mutations in FOXRED1 have been associated with Leigh syndrome and infantile-onset mitochondrial encephalopathy.

Calcium-binding mitochondrial carrier protein Aralar1 is a protein that in humans is encoded by the SLC25A12 gene. Aralar is an integral membrane protein located in the inner mitochondrial membrane. Its primary function as an antiporter is the transport of cytoplasmic glutamate with mitochondrial aspartate across the inner mitochondrial membrane, dependent on the binding of one calcium ion. Mutations in this gene cause early infantile epileptic encephalopathy 39 (EIEE39), symptomized by global hypomyelination of the central nervous system, refractory seizures, and neurodevelopmental impairment. This gene has connections to autism.
Phenylalanyl-tRNA synthetase, mitochondrial (FARS2) is an enzyme that in humans is encoded by the FARS2 gene. This protein encoded by FARS2 localizes to the mitochondrion and plays a role in mitochondrial protein translation. Mutations in this gene have been associated with combined oxidative phosphorylation deficiency 14, also known as Alpers encephalopathy, as well as spastic paraplegia 77 and infantile-onset epilepsy and cytochrome c oxidase deficiency.

Mitochondrial import inner membrane translocase subunit TIM50 is a protein that in humans is encoded by the TIMM50 gene. Tim50 is a subunit of the Tim23 translocase complex in the inner mitochondrial membrane. Mutations in TIMM50 can lead to epilepsy, severe intellectual disability, and 3-methylglutaconic aciduria. TIMM50 expression is increased in breast cancer cells and decreased in hypertrophic hearts.
Mitochondrially encoded tRNA phenylalanine also known as MT-TF is a transfer RNA which in humans is encoded by the mitochondrial MT-TF gene.
Mitochondrially encoded tRNA threonine also known as MT-TT is a transfer RNA which in humans is encoded by the mitochondrial MT-TT gene.
Early myoclonic encephalopathy (EME) is a rare neonatal-onset epilepsy developmental and epileptic encephalopathy (DEE) with an onset at neonatal period or during the first 3 months of life. It is marked by the presence of myoclonic seizures but multiple seizure types may occur. The electroencephalographic recording is abnormal with eitherusually a suppression-burst pattern or other significantly abnormal patterns. On most occasions the seizures are drug-resistant. After several months, the seizure pattern may develop into infantile spasms syndrome. The neurological exam is abnormal with a significant risk of early death. Various genetic and metabolic disorders are responsible. At present, EME and Ohtahara syndrome are recorded as distinct patterns in the categorization of epilepsies but both neonatal-onset epilepsy syndromes are considered to be merged in one unique entity. It is a severe type of epilepsy syndrome associated with high level of resistance to treatment and a high risk for cognitive impairment. The myoclonic seizures could be seen in other epilepsy syndromes. Multiple types of childhood epilepsies are usually mentioned as myoclonic epilepsies when the myoclonic seizures are a predominant feature.

Serine active site-containing protein 1, or Protein SERAC1 is a protein in humans that is encoded by the SERAC1 gene. The protein encoded by this gene is a phosphatidylglycerol remodeling protein found at the interface of mitochondria and endoplasmic reticula, where it mediates phospholipid exchange. The encoded protein plays a major role in mitochondrial function and intracellular cholesterol trafficking. Defects in this gene are a cause of 3-methylglutaconic aciduria with deafness, encephalopathy, and Leigh-like syndrome (MEGDEL). Two transcript variants, one protein-coding and the other non-protein coding, have been found for this gene.

Solute carrier family 13 (sodium-dependent citrate transporter), member 5 also known as the Na+/citrate cotransporter or mIndy is a protein that in humans is encoded by the SLC13A5 gene. It is the mammalian homolog of the fly Indy gene.

NADH:ubiquinone oxidoreductase complex assembly factor 4, (NDUFAF4) also known as Hormone-regulated proliferation-associated protein of 20 kDa, (HRPAP20) or C6orf66 is a protein that in humans is encoded by the NDUFAF4 gene. NDUFAF4 is a mitochondrial assembly protein involved in the assembly of NADH dehydrogenase (ubiquinone) also known as complex I, which is located in the mitochondrial inner membrane and is the largest of the five complexes of the electron transport chain. Mutations in this gene have been associated with complex I deficiency and infantile mitochondrial encephalomyopathy. Elevations in HRPAP20 have also been implicated in breast cancer.

Solute carrier family 25 member 46 is a protein that in humans is encoded by the SLC25A46 gene. This protein is a member of the SLC25 mitochondrial solute carrier family. It is a transmembrane protein located in the mitochondrial outer membrane involved in lipid transfer from the endoplasmic reticulum (ER) to mitochondria. Mutations in this gene result in neuropathy and optic atrophy.
SLC13A5 citrate transporter disorder is a rare neurological disease, also known as SLC13A5 epilepsy and by other names. It is a spectrum disorder, discovered in 2014. It is one of the many subtypes of Ohtahara syndrome that have been linked to metabolic causes.