Related Research Articles

Leptin, also known as obese protein, is a protein hormone predominantly made by adipocytes. Its primary role is likely to regulate long-term energy balance.

Adipose tissue is a loose connective tissue composed mostly of adipocytes. It also contains the stromal vascular fraction (SVF) of cells including preadipocytes, fibroblasts, vascular endothelial cells and a variety of immune cells such as adipose tissue macrophages. Its main role is to store energy in the form of lipids, although it also cushions and insulates the body.
Basal metabolic rate (BMR) is the rate of energy expenditure per unit time by endothermic animals at rest. It is reported in energy units per unit time ranging from watt (joule/second) to ml O2/min or joule per hour per kg body mass J/(h·kg). Proper measurement requires a strict set of criteria to be met. These criteria include being in a physically and psychologically undisturbed state and being in a thermally neutral environment while in the post-absorptive state (i.e., not actively digesting food). In bradymetabolic animals, such as fish and reptiles, the equivalent term standard metabolic rate (SMR) applies. It follows the same criteria as BMR, but requires the documentation of the temperature at which the metabolic rate was measured. This makes BMR a variant of standard metabolic rate measurement that excludes the temperature data, a practice that has led to problems in defining "standard" rates of metabolism for many mammals.

Adipocytes, also known as lipocytes and fat cells, are the cells that primarily compose adipose tissue, specialized in storing energy as fat. Adipocytes are derived from mesenchymal stem cells which give rise to adipocytes through adipogenesis. In cell culture, adipocyte progenitors can also form osteoblasts, myocytes and other cell types.

Neuropeptide Y (NPY) is a 36 amino-acid neuropeptide that is involved in various physiological and homeostatic processes in both the central and peripheral nervous systems. It is secreted alongside other neurotransmitters such as GABA and glutamate.

Weight gain is an increase in body weight. This can involve an increase in muscle mass, fat deposits, excess fluids such as water or other factors. Weight gain can be a symptom of a serious medical condition.
Calorie restriction is a dietary regimen that reduces the energy intake from foods and beverages without incurring malnutrition. The possible effect of calorie restriction on body weight management, longevity, and aging-associated diseases has been an active area of research.

A very-low-calorie diet (VLCD), also known as semistarvation diet and crash diet, is a type of diet with very or extremely low daily food energy consumption. VLCDs are defined as a diet of 800 kilocalories (3,300 kJ) per day or less. Modern medically supervised VLCDs use total meal replacements, with regulated formulations in Europe and Canada which contain the recommended daily requirements for vitamins, minerals, trace elements, fatty acids, protein and electrolyte balance. Carbohydrates may be entirely absent, or substituted for a portion of the protein; this choice has important metabolic effects. Medically supervised VLCDs have specific therapeutic applications for rapid weight loss, such as in morbid obesity or before a bariatric surgery, using formulated, nutritionally complete liquid meals containing 800 kilocalories or less per day for a maximum of 12 weeks.
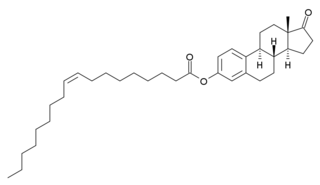
Oleoyl-estrone (OE), or estrone 3-oleate, is a fatty acid ester of estrone. It is a naturally circulating hormone in animals, including humans. It was studied as a potential weight-loss drug, but failed to show benefit in clinical trials. It was first reported in 1996 to cause a body fat loss effect in rats in the International Journal of Obesity and Related Metabolic Disorders. The animal research has all been conducted by the Nitrogen-Obesity Research Group of the University of Barcelona.

Jeffrey M. Friedman is a molecular geneticist at New York City's Rockefeller University and an Investigator of the Howard Hughes Medical Institute. His discovery of the hormone leptin and its role in regulating body weight has had a major role in the area of human obesity. Friedman is a physician scientist studying the genetic mechanisms that regulate body weight. His research on various aspects of obesity received national attention in late 1994, when it was announced that he and his colleagues had isolated the mouse ob gene and its human homologue. They subsequently found that injections of the encoded protein, leptin, decreases body weight of mice by reducing food intake and increasing energy expenditure. Current research is aimed at understanding the genetic basis of obesity in human and the mechanisms by which leptin transmits its weight-reducing signal.
Nesfatin-1 is a neuropeptide produced in the hypothalamus of mammals. It participates in the regulation of hunger and fat storage. Increased nesfatin-1 in the hypothalamus contributes to diminished hunger, a 'sense of fullness', and a potential loss of body fat and weight.

The central melanocortin system is defined anatomically as a collection of central nervous system circuits which include:
In biology, energy homeostasis, or the homeostatic control of energy balance, is a biological process that involves the coordinated homeostatic regulation of food intake and energy expenditure. The human brain, particularly the hypothalamus, plays a central role in regulating energy homeostasis and generating the sense of hunger by integrating a number of biochemical signals that transmit information about energy balance. Fifty percent of the energy from glucose metabolism is immediately converted to heat.
Hunger is a sensation that motivates the consumption of food. The sensation of hunger typically manifests after only a few hours without eating and is generally considered to be unpleasant. Satiety occurs between 5 and 20 minutes after eating. There are several theories about how the feeling of hunger arises. The desire to eat food, or appetite, is another sensation experienced with regard to eating.

Weight management refers to behaviors, techniques, and physiological processes that contribute to a person's ability to attain and maintain a healthy weight. Most weight management techniques encompass long-term lifestyle strategies that promote healthy eating and daily physical activity. Moreover, weight management involves developing meaningful ways to track weight over time and to identify the ideal body weights for different individuals.
Sleep is important in regulating metabolism. Mammalian sleep can be sub-divided into two distinct phases - REM and non-REM (NREM) sleep. In humans and cats, NREM sleep has four stages, where the third and fourth stages are considered slow-wave sleep (SWS). SWS is considered deep sleep, when metabolism is least active.

E-6837 is an orally active, 5-HT6 agonist developed in an attempt to create an anti-obesity medication. In cell lines expressing rat 5-HT6 receptors, it acted as a partial agonist (on presumed silent receptors), while it acted as a full agonist on human 5-HT6 receptors (which are constitutively active). Oral administration of E-6837 reduced food intake, but only transiently. In rats, twice daily administration of E-6837 over the course of 4 weeks resulted in a 15.7% reduction in body weight, compared to 11% reduction for sibutramine. This weight loss remained significant for E-6837 after a 43-day withdrawal period, whereas the weight difference was non-significant for sibutramine (i.e., sibutramine had a rebound effect while E-6837 did not), and this weight loss was found to be due to a loss of fat mass. The reduction in fat mass in E-6837 treated animals was associated with a 50% decrease in plasma leptin levels, and also reduced glucose and insulin levels in plasma after a glucose tolerance test. This indicates that weight loss from E-6837 is associated with improved insulin sensitivity, and thus, better glycemic control.
Ingestive behaviors encompass all eating and drinking behaviors. These actions are influenced by physiological regulatory mechanisms; these mechanisms exist to control and establish homeostasis within the human body. Disruptions in these ingestive regulatory mechanisms can result in eating disorders such as obesity, anorexia, and bulimia.
Sleep and weight is the association between the amount of sleep an individual obtains and the weight of that individual.

Pathophysiology of obesity is the study of disordered physiological processes that cause, result from, or are otherwise associated with obesity. A number of possible pathophysiological mechanisms have been identified which may contribute in the development and maintenance of obesity.
References
- 1 2 3 Harris, R. B. (December 1990). "Role of set-point theory in regulation of body weight". FASEB Journal. 4 (15): 3310–3318. doi: 10.1096/fasebj.4.15.2253845 . PMID 2253845. S2CID 21297643.
- 1 2 3 Keesey, Richard E.; Hirvonen, Matt D. (1 September 1997). "Body Weight Set-Points: Determination and Adjustment". The Journal of Nutrition. 127 (9): 1875S–1883S. doi: 10.1093/jn/127.9.1875S . PMID 9278574.
- 1 2 Ghanemi A, Yoshioka M, St-Amand J (2018). "Broken Energy Homeostasis and Obesity Pathogenesis: The Surrounding Concepts". J Clin Med. 7 (11): 453. doi: 10.3390/jcm7110453 . PMC 6262529 . PMID 30463389.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - 1 2 3 4 5 6 7 8 9 Speakman, John R.; Levitsky, David A.; Allison, David B.; Bray, Molly S.; Castro, John M. de; Clegg, Deborah J.; Clapham, John C.; Dulloo, Abdul G.; Gruer, Laurence; Haw, Sally; Hebebrand, Johannes; Hetherington, Marion M.; Higgs, Susanne; Jebb, Susan A.; Loos, Ruth J. F.; Luckman, Simon; Luke, Amy; Mohammed-Ali, Vidya; O’Rahilly, Stephen; Pereira, Mark; Perusse, Louis; Robinson, Tom N.; Rolls, Barbara; Symonds, Michael E.; Westerterp-Plantenga, Margriet S. (1 November 2011). "Set points, settling points and some alternative models: theoretical options to understand how genes and environments combine to regulate body adiposity". Disease Models & Mechanisms. 4 (6): 733–745. doi: 10.1242/dmm.008698 . PMC 3209643 . PMID 22065844.
- ↑ Schwartz MW, Seeley RJ, Zeltser LM, Drewnowski A, Ravussin E, Redman LM; et al. (2017). "Obesity Pathogenesis: An Endocrine Society Scientific Statement". Endocr Rev. 38 (4): 267–296. doi:10.1210/er.2017-00111. PMC 5546881 . PMID 28898979.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Müller, Manfred J; Bosy-Westphal, Anja; Heymsfield, Steven B (2010-08-09). "Is there evidence for a set point that regulates human body weight?". F1000 Medicine Reports. 2: 59. doi: 10.3410/M2-59 . ISSN 1757-5931. PMC 2990627 . PMID 21173874.
- ↑ Keys, A.; Brožek, J.; Henschel, A.; Mickelsen, O.; Taylor, H. L. (1950). The Biology of Human Starvation (2 volumes). St. Paul, MN: University of Minnesota Press, MINNE edition. ISBN 978-0-8166-7234-9.[ page needed ]
- ↑ Bernardis, Lee L.; McEwent, Geraldine; Kodis, Marjorie (1 September 1986). "Body weight set point studies in weanling rats with dorsomedial hypothalamic lesions (DMNL rats)". Brain Research Bulletin. 17 (3): 451–460. doi:10.1016/0361-9230(86)90254-6. PMID 3533223. S2CID 4765497.
- ↑ Davis, Jon F.; Choi, Derrick L.; Schurdak, Jennifer D.; Fitzgerald, Maureen F.; Clegg, Deborah J.; Lipton, Jack W.; Figlewicz, Dianne P.; Benoit, Stephen C. (1 April 2011). "Leptin Regulates Energy Balance and Motivation Through Action at Distinct Neural Circuits". Biological Psychiatry. 69 (7): 668–674. doi:10.1016/j.biopsych.2010.08.028. PMC 3058141 . PMID 21035790.