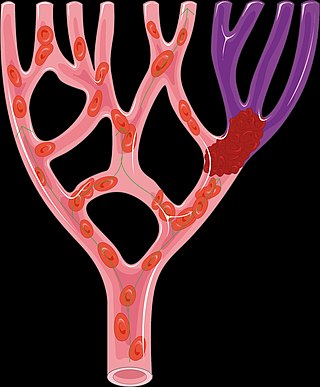
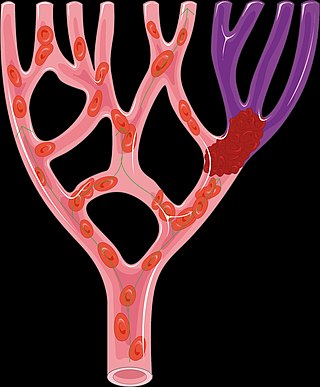
Thrombosis is the formation of a blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel is injured, the body uses platelets (thrombocytes) and fibrin to form a blood clot to prevent blood loss. Even when a blood vessel is not injured, blood clots may form in the body under certain conditions. A clot, or a piece of the clot, that breaks free and begins to travel around the body is known as an embolus.

A thrombus, colloquially called a blood clot, is the final product of the blood coagulation step in hemostasis. There are two components to a thrombus: aggregated platelets and red blood cells that form a plug, and a mesh of cross-linked fibrin protein. The substance making up a thrombus is sometimes called cruor. A thrombus is a healthy response to injury intended to stop and prevent further bleeding, but can be harmful in thrombosis, when a clot obstructs blood flow through healthy blood vessels in the circulatory system.

Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism. Ischemia is generally caused by problems with blood vessels, with resultant damage to or dysfunction of tissue i.e. hypoxia and microvascular dysfunction. It also implies local hypoxia in a part of a body resulting from constriction. Ischemia causes not only insufficiency of oxygen, but also reduced availability of nutrients and inadequate removal of metabolic wastes. Ischemia can be partial or total blockage. The inadequate delivery of oxygenated blood to the organs must be resolved either by treating the cause of the inadequate delivery or reducing the oxygen demand of the system that needs it. For example, patients with myocardial ischemia have a decreased blood flow to the heart and are prescribed with medications that reduce chronotrophy and ionotrophy to meet the new level of blood delivery supplied by the stenosed vasculature so that it is adequate.

Thrombolysis, also called fibrinolytic therapy, is the breakdown (lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and in cases of severe venous thromboembolism.
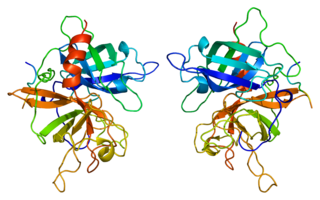
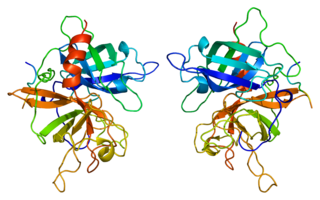
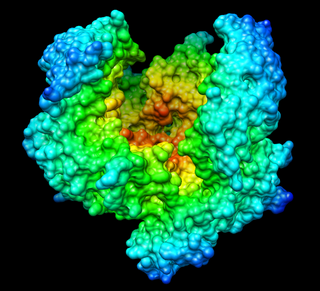
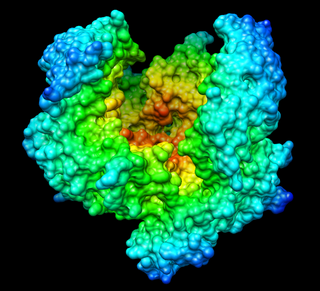
Tissue-type plasminogen activator, short name tPA, is a protein that facilitates the breakdown of blood clots. It acts as an enzyme to convert plasminogen into its active form plasmin, the major enzyme responsible for clot breakdown. It is a serine protease found on endothelial cells lining the blood vessels. Human tPA is encoded by the PLAT gene, and has a molecular weight of ~70 kDa in the single-chain form.

Stroke is a medical condition in which poor blood flow to the brain causes cell death. There are two main types of stroke: ischemic, due to lack of blood flow, and hemorrhagic, due to bleeding. Both cause parts of the brain to stop functioning properly.
Streptokinase is a thrombolytic medication activating plasminogen by nonenzymatic mechanism. As a medication it is used to break down clots in some cases of myocardial infarction, pulmonary embolism, and arterial thromboembolism. The type of heart attack it is used in is an ST elevation myocardial infarction (STEMI). It is given by injection into a vein.
Mechanical thrombectomy, or simply thrombectomy, is the removal of a blood clot (thrombus) from a blood vessel, often and especially endovascularly as an interventional radiology procedure called endovascular thrombectomy (EVT). It thus contrasts with thrombolysis by thrombolytic medications, as either alternative or complement thereto. It is commonly performed in the cerebral arteries as treatment to reverse the ischemia in some ischemic strokes. Open vascular surgery versions of thrombectomy also exist. The effectiveness of thrombectomy for strokes was confirmed in several randomised clinical trials conducted at various medical centers throughout the United States, as reported in a seminal multistudy report in 2015.
Alteplase, sold under the brand name Activase among others, is a biosynthetic form of human tissue-type plasminogen activator (t-PA). It is a thrombolytic medication used to treat acute ischemic stroke, acute ST-elevation myocardial infarction, pulmonary embolism associated with low blood pressure, and blocked central venous catheter. It is given by injection into a vein or artery. Alteplase is the same as the normal human plasminogen activator produced in vascular endothelial cells and is synthesized via recombinant DNA technology in Chinese hamster ovary cells (CHO). Alteplase causes the breakdown of a clot by inducing fibrinolysis.

Desmoteplase is a novel, highly fibrin-specific "clot-busting" (thrombolytic) drug in development that reached phase III clinical trials. The Danish pharmaceutical company, Lundbeck, owns the worldwide rights to Desmoteplase. In 2009, two large trials were started to test it as a safe and effective treatment for patients with acute ischaemic stroke. After disappointing results in DIAS-3, DIAS-4 was terminated, and in December 2014 Lundbeck announced that they would stop the development of desmoteplase.

Cerebral infarction is the pathologic process that results in an area of necrotic tissue in the brain. It is caused by disrupted blood supply (ischemia) and restricted oxygen supply (hypoxia), most commonly due to thromboembolism, and manifests clinically as ischemic stroke. In response to ischemia, the brain degenerates by the process of liquefactive necrosis.
Anistreplase is a thrombolytic drug. It is also known as anisoylated plasminogen streptokinase activator complex (APSAC). As a thrombolytic drug, it is used to treat blood clots in emergency situations.
Tenecteplase, sold under the trade names TNKase, Metalyse and Elaxim, is an enzyme used as a thrombolytic drug.

Désiré, Baron Collen is a Belgian physician, chemist, biotechnology entrepreneur and life science investor. He made several discoveries in thrombosis, haemostasis and vascular biology in many of which serendipity played a significant role. His main achievement has been his role in the development of tissue-type plasminogen activator (t-PA) from a laboratory concept to a life-saving drug for dissolving blood clots causing acute myocardial infarction or acute ischemic stroke. Recombinant t-PA was produced and marketed by Genentech Inc as Activase and by Boehringer Ingelheim GmbH as Actilyse, and is considered biotechnology's first life saving drug.
The National Institutes of Health Stroke Scale, or NIH Stroke Scale (NIHSS), is a tool used by healthcare providers to objectively quantify the impairment caused by a stroke and aid planning post-acute care disposition, though was intended to assess differences in interventions in clinical trials. The NIHSS was designed for the National Institute of Neurological Disorders and Stroke (NINDS) Recombinant Tissue Plasminogen Activator (rt-PA) for Acute Stroke Trial and was first published by neurologist Dr. Patrick Lyden and colleagues in 2001. Prior to the NIHSS, during the late 1980s, several stroke-deficit rating scales were in use.

Acute limb ischaemia (ALI) occurs when there is a sudden lack of blood flow to a limb, within 14 days of symptoms onset. It is different from another condition which is more chronic called critical limb ischemia (CLD). CLD is the end stage of peripheral vascular disease where there is still some collateral circulation (alternate circulation pathways} that bring some blood to the distal parts of the limbs. While limbs in both acute and chronic limb ischemia may be pulseless, a chronically ischemic limb is typically warm and pink due to a well-developed collateral artery network and does not need emergency intervention to avoid limb loss.

Reperfusion therapy is a medical treatment to restore blood flow, either through or around, blocked arteries, typically after a heart attack. Reperfusion therapy includes drugs and surgery. The drugs are thrombolytics and fibrinolytics used in a process called thrombolysis. Surgeries performed may be minimally-invasive endovascular procedures such as a percutaneous coronary intervention (PCI), which involves coronary angioplasty. The angioplasty uses the insertion of a balloon and/or stents to open up the artery. Other surgeries performed are the more invasive bypass surgeries that graft arteries around blockages.

The MERCI Retriever is a medical device designed to treat Ischemic Strokes. The name is an acronym for Mechanical Embolus Removal in Cerebral Ischemia. Designed by University of California, Los Angeles in 2001, MERCI was the first device approved in the U.S. to remove blood clots in patients who had acute brain ischemia.
Thrombus perviousness is an imaging biomarker which is used to estimate clot permeability from CT imaging. It reflects the ability of artery-occluding thrombi to let fluid seep into and through them. The more pervious a thrombus, the more fluid it lets through. Thrombus perviousness can be measured using radiological imaging routinely performed in the clinical management of acute ischemic stroke: CT scans without intravenous contrast combined with CT scans after intravenously administered contrast fluid. Pervious thrombi may let more blood pass through to the ischemic brain tissue, and/or have a larger contact surface and histopathology more sensitive for thrombolytic medication. Thus, patients with pervious thrombi may have less brain tissue damage by stroke. The value of thrombus perviousness in acute ischemic stroke treatment is currently being researched.
Hemorrhagic transformation (HT) or hemorrhagic conversion is a medical complication that can occur in the brain following an acute ischemic stroke, a condition in which blood flow to the brain is blocked.