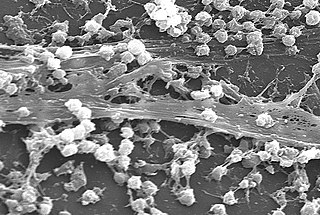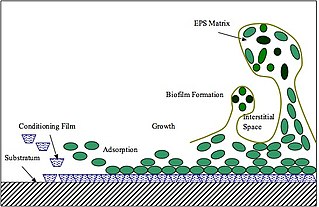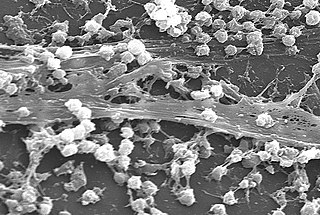
A biofilm is an syntrophic community of microorganisms in which cells stick to each other and often also to a surface. These adherent cells become embedded within a slimy extracellular matrix that is composed of extracellular polymeric substances (EPSs). The cells within the biofilm produce the EPS components, which are typically a polymeric combination of extracellular polysaccharides, proteins, lipids and DNA. Because they have three-dimensional structure and represent a community lifestyle for microorganisms, they have been metaphorically described as "cities for microbes".

In dentistry, calculus or tartar is a form of hardened dental plaque. It is caused by precipitation of minerals from saliva and gingival crevicular fluid (GCF) in plaque on the teeth. This process of precipitation kills the bacterial cells within dental plaque, but the rough and hardened surface that is formed provides an ideal surface for further plaque formation. This leads to calculus buildup, which compromises the health of the gingiva (gums). Calculus can form both along the gumline, where it is referred to as supragingival, and within the narrow sulcus that exists between the teeth and the gingiva, where it is referred to as subgingival.
Teeth cleaning is part of oral hygiene and involves the removal of dental plaque from teeth with the intention of preventing cavities, gingivitis, and periodontal disease. People routinely clean their own teeth by brushing and interdental cleaning, and dental hygienists can remove hardened deposits (tartar) not removed by routine cleaning. Those with dentures and natural teeth may supplement their cleaning with a denture cleaner.

Tooth decay, also known as cavities or caries, is the breakdown of teeth due to acids produced by bacteria. The cavities may be a number of different colors from yellow to black. Symptoms may include pain and difficulty with eating. Complications may include inflammation of the tissue around the tooth, tooth loss and infection or abscess formation.

Streptococcus mutans is a facultatively anaerobic, gram-positive coccus commonly found in the human oral cavity and is a significant contributor to tooth decay. It is part of the "streptococci", an informal general name for all species in the genus Streptococcus. The microbe was first described by James Kilian Clarke in 1924.
Dental plaque is a biofilm of microorganisms that grows on surfaces within the mouth. It is a sticky colorless deposit at first, but when it forms tartar, it is often brown or pale yellow. It is commonly found between the teeth, on the front of teeth, behind teeth, on chewing surfaces, along the gumline (supragingival), or below the gumline cervical margins (subgingival). Dental plaque is also known as microbial plaque, oral biofilm, dental biofilm, dental plaque biofilm or bacterial plaque biofilm. Bacterial plaque is one of the major causes for dental decay and gum disease.
The dental pellicle, or acquired pellicle, is a protein film that forms on the surface enamel, dentin, artificial crowns, and bridges by selective binding of glycoproteins from saliva that prevents continuous deposition of salivary calcium phosphate. It forms in seconds after a tooth is cleaned, or after chewing. It protects the tooth from the acids produced by oral microorganisms after consuming carbohydrates.

Early childhood caries (ECC), formerly known as nursing bottle caries, baby bottle tooth decay, night bottle mouth and night bottle caries, is a disease that affects teeth in children aged between birth and 71 months. ECC is characterized by the presence of 1 or more decayed, missing, or filled tooth surfaces in any primary tooth. ECC has been shown to be a very common, transmissible bacterial infection, usually passed from the primary caregiver to the child. The main bacteria responsible for dental cavities are Streptococcus mutans (S.mutans) and Lactobacillus. There is also evidence that supports that those who are in lower socioeconomic populations are at greater risk of developing ECC.
Streptococcus sanguinis, formerly known as Streptococcus sanguis, is a Gram-positive facultative anaerobic coccus species of bacteria and a member of the Viridans Streptococcus group. S. sanguinis is a normal inhabitant of the healthy human mouth where it is particularly found in dental plaque, where it modifies the environment to make it less hospitable for other strains of Streptococcus that cause cavities, such as Streptococcus mutans.

Streptococcus oralis is a Gram positive viridans streptococcus of the Streptococcus mitis group. S. oralis is one of the pioneer species associated with eubiotic dental pellicle biofilms, and can be found in high numbers on most oral surfaces. It has been, however, found to be an opportunistic pathogen as well.
Porphyromonas gingivalis belongs to the phylum Bacteroidota and is a nonmotile, Gram-negative, rod-shaped, anaerobic, pathogenic bacterium. It forms black colonies on blood agar.
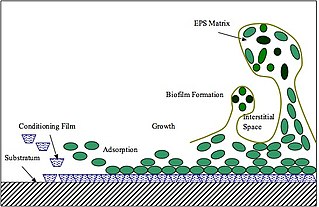
Extracellular polymeric substances (EPSs) are natural polymers of high molecular weight secreted by microorganisms into their environment. EPSs establish the functional and structural integrity of biofilms, and are considered the fundamental component that determines the physicochemical properties of a biofilm. EPS in the matrix of biofilms provides compositional support and protection of microbial communities from the harsh environments. Components of EPS can be of different classes of polysaccharides, lipids, nucleic acids, proteins, lipopolysaccharides, and minerals.

Oral microbiology is the study of the microorganisms (microbiota) of the oral cavity and their interactions between oral microorganisms or with the host. The environment present in the human mouth is suited to the growth of characteristic microorganisms found there. It provides a source of water and nutrients, as well as a moderate temperature. Resident microbes of the mouth adhere to the teeth and gums to resist mechanical flushing from the mouth to stomach where acid-sensitive microbes are destroyed by hydrochloric acid.

Oral hygiene is the practice of keeping one's oral cavity clean and free of disease and other problems by regular brushing of the teeth and adopting good hygiene habits. It is important that oral hygiene be carried out on a regular basis to enable prevention of dental disease and bad breath. The most common types of dental disease are tooth decay and gum diseases, including gingivitis, and periodontitis.

Tooth remineralization is the natural repair process for non-cavitated tooth lesions, in which calcium, phosphate and sometimes fluoride ions are deposited into crystal voids in demineralised enamel. Remineralization can contribute towards restoring strength and function within tooth structure.
Oral ecology is the microbial ecology of the microorganisms found in mouths. Oral ecology, like all forms of ecology, involves the study of the living things found in oral cavities as well as their interactions with each other and with their environment. Oral ecology is frequently investigated from the perspective of oral disease prevention, often focusing on conditions such as dental caries, candidiasis ("thrush"), gingivitis, periodontal disease, and others. However, many of the interactions between the microbiota and oral environment protect from disease and support a healthy oral cavity. Interactions between microbes and their environment can result in the stabilization or destabilization of the oral microbiome, with destabilization believed to result in disease states. Destabilization of the microbiome can be influenced by several factors, including diet changes, drugs or immune system disorders.
Periodontal pathogens are bacteria that have been shown to significantly contribute to periodontitis.
Corynebacterium matruchotii is a species of bacteria in the genus Corynebacterium. Corynebacteria occur within the normal flora of the human body.
Plaque hypotheses are theories to explain the role of plaque bacteria in dental caries and in periodontitis. They rely heavily on the postulates of Koch and on the work of Louis Pasteur (1822–1895). Changing perceptions have altered treatment models.

Jessica A. Scoffield is an American microbiologist and an assistant professor in the Department of Microbiology at the University of Alabama at Birmingham School of Medicine. Scoffield studies the mechanisms by which oral commensal bacteria interfere with pathogenic bacterial growth in order to inform the development of active therapeutic tools to prevent drug resistant pathogen infection. In 2019, Scoffield became the inaugural recipient of the American Association for Dental Research Procter and Gamble Underrepresented Faculty Research Fellowship.