Related Research Articles

T cells are one of the important types of white blood cells of the immune system and play a central role in the adaptive immune response. T cells can be distinguished from other lymphocytes by the presence of a T-cell receptor (TCR) on their cell surface.
The regulatory T cells (Tregs or Treg cells), formerly known as suppressor T cells, are a subpopulation of T cells that modulate the immune system, maintain tolerance to self-antigens, and prevent autoimmune disease. Treg cells are immunosuppressive and generally suppress or downregulate induction and proliferation of effector T cells. Treg cells express the biomarkers CD4, FOXP3, and CD25 and are thought to be derived from the same lineage as naïve CD4+ cells. Because effector T cells also express CD4 and CD25, Treg cells are very difficult to effectively discern from effector CD4+, making them difficult to study. Research has found that the cytokine transforming growth factor beta (TGF-β) is essential for Treg cells to differentiate from naïve CD4+ cells and is important in maintaining Treg cell homeostasis.
Alloimmunity is an immune response to nonself antigens from members of the same species, which are called alloantigens or isoantigens. Two major types of alloantigens are blood group antigens and histocompatibility antigens. In alloimmunity, the body creates antibodies against the alloantigens, attacking transfused blood, allotransplanted tissue, and even the fetus in some cases. Alloimmune (isoimmune) response results in graft rejection, which is manifested as deterioration or complete loss of graft function. In contrast, autoimmunity is an immune response to the self's own antigens. Alloimmunization (isoimmunization) is the process of becoming alloimmune, that is, developing the relevant antibodies for the first time.

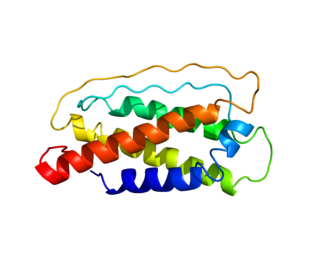
FOXP3, also known as scurfin, is a protein involved in immune system responses. A member of the FOX protein family, FOXP3 appears to function as a master regulator of the regulatory pathway in the development and function of regulatory T cells. Regulatory T cells generally turn the immune response down. In cancer, an excess of regulatory T cell activity can prevent the immune system from destroying cancer cells. In autoimmune disease, a deficiency of regulatory T cell activity can allow other autoimmune cells to attack the body's own tissues.
Interleukin 7 (IL-7) is a protein that in humans is encoded by the IL7 gene.
Immune tolerance, or immunological tolerance, or immunotolerance, is a state of unresponsiveness of the immune system to substances or tissue that would otherwise have the capacity to elicit an immune response in a given organism. It is induced by prior exposure to that specific antigen and contrasts with conventional immune-mediated elimination of foreign antigens. Tolerance is classified into central tolerance or peripheral tolerance depending on where the state is originally induced—in the thymus and bone marrow (central) or in other tissues and lymph nodes (peripheral). The mechanisms by which these forms of tolerance are established are distinct, but the resulting effect is similar.
In immunology, a naive T cell (Th0 cell) is a T cell that has differentiated in the thymus, and successfully undergone the positive and negative processes of central selection in the thymus. Among these are the naive forms of helper T cells (CD4+) and cytotoxic T cells (CD8+). Any naive T cell is considered immature and, unlike activated or memory T cells, has not encountered its cognate antigen within the periphery. After this encounter, the naive T cell is considered a mature T cell.

Integrin, alpha E (ITGAE) also known as CD103 is an integrin protein that in human is encoded by the ITGAE gene. CD103 binds integrin beta 7 to form the complete heterodimeric integrin molecule αEβ7, which has no distinct name. The αEβ7 complex is often referred to as "CD103" though this strictly refers only to the αE chain. Note that the β7 subunit can bind with other integrin α chains, such as α4 (CD49d).

Probable G-protein coupled receptor 83 is a protein that in humans is encoded by the GPR83 gene.

Lymphocyte-activation gene 3, also known as LAG-3, is a protein which in humans is encoded by the LAG3 gene. LAG3, which was discovered in 1990 and was designated CD223 after the Seventh Human Leucocyte Differentiation Antigen Workshop in 2000, is a cell surface molecule with diverse biologic effects on T cell function. It is an immune checkpoint receptor and as such is the target of various drug development programs by pharmaceutical companies seeking to develop new treatments for cancer and autoimmune disorders. In soluble form it is also being developed as a cancer drug in its own right.

Fibrinogen-like protein 2, also known as FGL2, is a protein which in humans is encoded by the FGL2 gene.

Zinc finger protein Helios is a protein that in humans is encoded by the IKZF2 gene. This protein is a member of Ikaros family of transcription factors.

Tumor necrosis factor receptor superfamily member 18 (TNFRSF18), also known as glucocorticoid-induced TNFR-related protein (GITR) or CD357. GITR is encoded and tnfrsf18 gene at chromosome 4 in mice. GITR is type I transmembrane protein and is described in 4 different isoforms. GITR human orthologue, also called activation-inducible TNFR family receptor (AITR), is encoded by the TNFRSF18 gene at chromosome 1.

Interleukin-2 receptor alpha chain is a protein involved in assembly of high-affinity Interleukin-2 receptor, consisting of alpha (IL2RA), beta (IL2RB) and the common gamma chain (IL2RG). As the name indicates, this receptor interacts with pleiotropic cytokine called Interleukin-2, which effect is mainly important for immune homeostasis.
T helper 3 cells (Th3) are a subset of T lymphocytes with immunoregulary and immunosuppressive functions, that can be induced by administration of foreign oral antigen. Th3 cells act mainly through the secretion of anti-inflammatory cytokine transforming growth factor beta (TGF-β). Th3 have been described both in mice and human as CD4+FOXP3− regulatory T cells. Th3 cells were first described in research focusing on oral tolerance in the experimental autoimmune encephalitis (EAE) mouse model and later described as CD4+CD25−FOXP3−LAP+ cells, that can be induced in the gut by oral antigen through T cell receptor (TCR) signalling.

Follicular helper T cells (also known as follicular B helper T cells and abbreviated as TFH), are antigen-experienced CD4+ T cells found in the periphery within B cell follicles of secondary lymphoid organs such as lymph nodes, spleen and Peyer's patches, and are identified by their constitutive expression of the B cell follicle homing receptor CXCR5. Upon cellular interaction and cross-signaling with their cognate follicular (Fo B) B cells, TFH cells trigger the formation and maintenance of germinal centers through the expression of CD40 ligand (CD40L) and the secretion of IL-21 and IL-4. TFH cells also migrate from T cell zones into these seeded germinal centers, predominantly composed of rapidly dividing B cells mutating their Ig genes. Within germinal centers, TFH cells play a critical role in mediating the selection and survival of B cells that go on to differentiate either into long-lived plasma cells capable of producing high affinity antibodies against foreign antigen, or germinal center-dependent memory B cells capable of quick immune re-activation in the future if ever the same antigen is re-encountered. TFH cells are also thought to facilitate negative selection of potentially autoimmune-causing mutated B cells in the germinal center. However, the biomechanisms by which TFH cells mediate germinal center tolerance are yet to be fully understood.

CD25 deficiency or interleukin 2 receptor alpha deficiency is an immunodeficiency disorder associated with mutations in the interleukin 2 receptor alpha (CD25) (IL2RA) gene. The mutations cause expression of a defective α chain or complete absence thereof, an essential part of high-affinity interleukin-2 (IL-2) receptors. The result is a syndrome described as IPEX-like or a SCID.
Type 1 regulatory cells or Tr1 (TR1) cells are a class of regulatory T cells participating in peripheral immunity as a subsets of CD4+ T cells. Tr1 cells regulate tolerance towards antigens of any origin. Tr1 cells are self or non-self antigen specific and their key role is to induce and maintain peripheral tolerance and suppress tissue inflammation in autoimmunity and graft vs. host disease.
Infectious tolerance is a term referring to a phenomenon where a tolerance-inducing state is transferred from one cell population to another. It can be induced in many ways; although it is often artificially induced, it is a natural in vivo process. A number of research deal with the development of a strategy utilizing this phenomenon in transplantation immunology. The goal is to achieve long-term tolerance of the transplant through short-term therapy.
Thymic epithelial cells (TECs) are specialized cells with high degree of anatomic, phenotypic and functional heterogeneity that are located in the outer layer (epithelium) of the thymic stroma. The thymus, as a primary lymphoid organ, mediates T cell development and maturation. The thymic microenvironment is established by TEC network filled with thymocytes in different developing stages. TECs and thymocytes are the most important components in the thymus, that are necessary for production of functionally competent T lymphocytes and self tolerance. Dysfunction of TECs causes several immunodeficiencies and autoimmune diseases.
References
- ↑ Negoro T, Iinuma F, Watanabe M (February 1996). "Cellular induction mechanism of CD8+ suppressor T cells by DMBA and TPA: formation of CD4+ suppressor-inducer T cells". Cell. Immunol. 167 (2): 216–23. doi:10.1006/cimm.1996.0029. PMID 8603430.
- ↑ Shevach EM, DiPaolo RA, Andersson J, Zhao DM, Stephens GL, Thornton AM (August 2006). "The lifestyle of naturally occurring CD4+ CD25+ Foxp3+ regulatory T cells". Immunol. Rev. 212: 60–73. doi:10.1111/j.0105-2896.2006.00415.x. PMID 16903906. S2CID 1711208.
- ↑ Mottet C, Golshayan D (November 2007). "CD4+CD25+Foxp3+ regulatory T cells: from basic research to potential therapeutic use". Swiss Med Wkly. 137 (45–46): 625–34. doi: 10.4414/smw.2007.11916 . PMID 18027108. S2CID 41378647.