Definitions
Three categories of transmission-based precautions have been designed with respect to the modes of transmission, namely Contact precautions, Droplet precautions, and Airborne precautions. For some diseases with multiple routes of transmission, more than one transmission-based precautions category may be used. When used either singly or in combination, they are always used in addition to standard precautions. [1]
Contact precautions

Contact precautions are intended to prevent transmission of infectious agents, including epidemiologically important microorganisms, which are spread by direct or indirect contact with the patient or the patient's environment. The specific agents and circumstance for which contact precautions are indicated are found in Appendix A of the 2007 CDC Guidance. [1] The application of contact precautions for patients infected or colonized with Multidrug-Resistant Organisms MDROs is described in the 2006 HICPAC/CDC MDRO guideline. [14] Contact precautions also apply where the presence of excessive wound drainage, fecal incontinence, or other discharges from the body suggest an increased potential for extensive environmental contamination and risk of transmission. A single-patient room is preferred for patients who require contact precautions. When a single-patient room is not available, consultation with infection control personnel is recommended to assess the various risks associated with other patient placement options (e.g., cohorting, keeping the patient with an existing roommate). In multi-patient rooms, >3 feet spatial separation between beds is advised to reduce the opportunities for inadvertent sharing of items between the infected/colonized patient and other patients. Healthcare personnel caring for patients on contact precautions wear a gown and gloves for all interactions that may involve contact with the patient or potentially contaminated areas in the patient's environment. Donning PPE upon room entry and discarding before exiting the patient room is done to contain pathogens, especially those that have been implicated in transmission through environmental contamination (e.g., VRE, C. difficile, noroviruses and other intestinal tract pathogens; RSV) [15] [16] [17] [18] [19] [20] [21]
Droplet precautions

As of 2020, the classification systems of routes of respiratory disease transmission are based on a conceptual division of large versus small droplets, as defined in the 1930s. [22]
Droplet precautions are intended to prevent transmission of certain pathogens spread through close respiratory or mucous membrane contact with respiratory secretions, namely respiratory droplets. Because certain pathogens do not remain infectious over long distances in a healthcare facility, special air handling and ventilation are not required to prevent droplet transmission. Infectious agents for which mere droplet precautions are indicated include B. pertussis , influenza virus, adenovirus, rhinovirus, N. meningitidis , and group A streptococcus (for the first 24 hours of antimicrobial therapy). A single patient room is preferred for patients who require droplet precautions. When a single-patient room is not available, consultation with infection control personnel is recommended to assess the various risks associated with other patient placement options (e.g., cohorting, keeping the patient with an existing roommate). Spatial separation of > 3 feet and drawing the curtain between patient beds is especially important for patients in multi-bed rooms with infections transmitted by the droplet route. Healthcare personnel wear a simple mask (a respirator is not necessary) for close contact with an infectious patient, which is generally donned upon room entry. Patients on droplet precautions who must be transported outside of the room should wear a mask if tolerated and follow Respiratory Hygiene/Cough Etiquette.[ citation needed ]
Airborne precautions
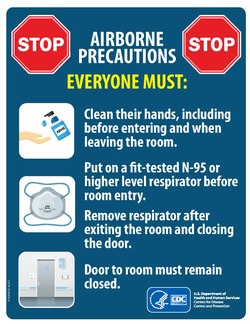
Airborne precautions prevent transmission of infectious agents that remain infectious over long distances when suspended in the air (e.g., rubeola virus [measles], varicella virus [chickenpox], M. tuberculosis, and SARS-CoV-2 [COVID-19]). The preferred placement for patients who require airborne precautions is in an airborne infection isolation room (AIIR). An AIIR is a single-patient room that is equipped with special air handling and ventilation capacity that meet the American Institute of Architects/Facility Guidelines Institute (AIA/FGI) standards for AIIRs (i.e., monitored negative pressure relative to the surrounding area, [23] air changes per hour (ach) for new construction and renovation and 6 air exchanges per hour for existing facilities, air exhausted directly to the outside or recirculated through HEPA filtration before return). [24] The Airborne Infectious Isolation Rooms are designed for prevention against the airborne diseases. They have their predefined Heating, Ventilation and Air conditioning (HVAC) criteria given by CDC, IDPH and ASHRAE Standard 170. CDC regulations only specify 12 ach and do not have any criteria on temperature or humidity. Meanwhile, IDPH/ASHRAE Standard 170 has more detailed design criteria for HVAC systems. According to their regulations the isolation rooms must have the ability to maintain the room temperature around 70F to 75F, while keeping the relative humidity (rh) to be minimum of 30% during winters and maximum of 60% during summers. The specified airflow is 12 ach total/ 2 ach OA (Outdoor Air) and the pressure should be negative relative to the adjacent spaces. There are some architectural design requirements for the rooms such as walls should be slab to slab, plaster or drywall ceilings with sliding-self-closing doors are preferred with all the leakages sealed. [25] The guidelines specified by CDC, IDPH/ASHRAE Standard 170 are focused on maintaining room temperatures within specified range, one thing to look into these conditions is how the relative humidity plays a role to effect the cooling systems used for maintaining the stringent temperature requirements. While the places with low relative humidity are perfectly fine with the evaporative cooling systems used in HVAC systems, but as the relative humidity pushes towards the higher ranges i.e. more than 60%, then the evaporative cooling systems fail miserably and have to be replaced with the refrigerated cooling systems. This is to be done to prevent the corrosive action of the moisture saturated on the corrosive surfaces of isolation rooms because evaporative cooling being slow in higher relative humidity areas will allow the more contact time between moisture and corrosive surfaces. For example, during the annual monsoon season in Arizona the cooling is going to be adversely affected due to high relative humidity. [26]
Some states require the availability of such rooms in hospitals, emergency departments, and nursing homes that care for patients with M. tuberculosis. A respiratory protection program that includes education about use of respirators, fit-testing, and user seal checks is required in any facility with AIIRs. In settings where airborne precautions cannot be implemented due to limited engineering resources (e.g., physician offices), masking the patient, placing the patient in a private room (e.g., office examination room) with the door closed, and providing N95 or higher level respirators or masks if respirators are not available for healthcare personnel will reduce the likelihood of airborne transmission until the patient is either transferred to a facility with an AIIR or returned to the home environment, as deemed medically appropriate. Healthcare personnel caring for patients on airborne precautions wear a mask or respirator, depending on the disease-specific recommendations (Appendix A), [1] that is donned prior to room entry. Whenever possible, non-immune HCWs should not care for patients with vaccine-preventable airborne diseases (e.g., measles, chickenpox, and smallpox).