Progressive multifocal leukoencephalopathy (PML) is a rare and often fatal viral disease characterized by progressive damage (-pathy) or inflammation of the white matter (leuko-) of the brain (-encephalo-) at multiple locations (multifocal). It is caused by the JC virus, which is normally present and kept under control by the immune system. The JC virus is harmless except in cases of weakened immune systems. In general, PML has a mortality rate of 30–50% in the first few months, and those who survive can be left with varying degrees of neurological disabilities.

Psoriasis is a long-lasting, noncontagious autoimmune disease characterized by raised areas of abnormal skin. These areas are red, or purple on some people with darker skin, dry, itchy, and scaly. Psoriasis varies in severity from small, localized patches to complete body coverage. Injury to the skin can trigger psoriatic skin changes at that spot, which is known as the Koebner phenomenon.
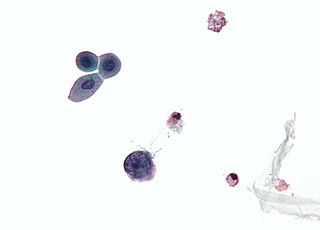
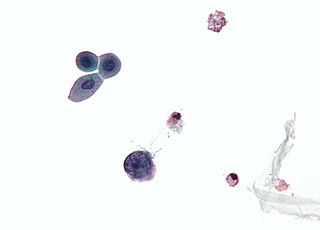
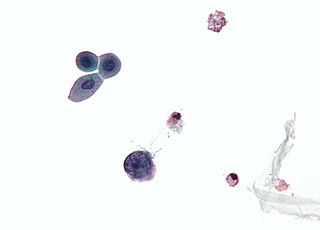
Polyomaviridae is a family of viruses whose natural hosts are primarily mammals and birds. As of 2020, there are six recognized genera and 117 species, five of which are unassigned to a genus. 14 species are known to infect humans, while others, such as Simian Virus 40, have been identified in humans to a lesser extent. Most of these viruses are very common and typically asymptomatic in most human populations studied. BK virus is associated with nephropathy in renal transplant and non-renal solid organ transplant patients, JC virus with progressive multifocal leukoencephalopathy, and Merkel cell virus with Merkel cell cancer.

Merkel cell carcinoma (MCC) is a rare and aggressive skin cancer occurring in about 3 people per 1,000,000 members of the population. It is also known as cutaneous APUDoma, primary neuroendocrine carcinoma of the skin, primary small cell carcinoma of the skin, and trabecular carcinoma of the skin. Factors involved in the development of MCC include the Merkel cell polyomavirus, a weakened immune system, and exposure to ultraviolet radiation. Merkel-cell carcinoma usually arises on the head, neck, and extremities, as well as in the perianal region and on the eyelid. It is more common in people over 60 years old, Caucasian people, and males. MCC is less common in children.

Pyoderma gangrenosum is a rare, inflammatory skin disease where painful pustules or nodules become ulcers that progressively grow. Pyoderma gangrenosum is not infectious.
The BK virus is a member of the polyomavirus family. Past infection with the BK virus is widespread, but significant consequences of infection are uncommon, with the exception of the immunocompromised and the immunosuppressed. BK virus is an abbreviation of the name of the first patient from whom the virus was isolated in 1971.

Solar urticaria (SU) is a rare condition in which exposure to ultraviolet or UV radiation, or sometimes even visible light, induces a case of urticaria or hives that can appear in both covered and uncovered areas of the skin. It is classified as a type of physical urticaria. The classification of disease types is somewhat controversial. One classification system distinguished various types of SU based on the wavelength of the radiation that causes the breakout; another classification system is based on the type of allergen that initiates a breakout.
Merkel cell polyomavirus was first described in January 2008 in Pittsburgh, Pennsylvania. It was the first example of a human viral pathogen discovered using unbiased metagenomic next-generation sequencing with a technique called digital transcriptome subtraction. MCV is one of seven currently known human oncoviruses. It is suspected to cause the majority of cases of Merkel cell carcinoma, a rare but aggressive form of skin cancer. Approximately 80% of Merkel cell carcinoma (MCC) tumors have been found to be infected with MCV. MCV appears to be a common—if not universal—infection of older children and adults. It is found in respiratory secretions suggesting that it may be transmitted by a respiratory route. But it also can be found shedding from healthy skin, and in gastrointestinal tract tissues and elsewhere, and so its precise mode of transmission remains unknown. In addition, recent studies suggest that this virus may latently infect the human sera and PBMCs.
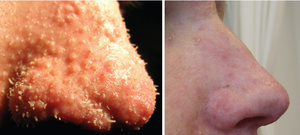
Trichodysplasia spinulosa polyomavirus is a member virus of Human polyomavirus 8 that infects human hosts. First discovered in 2010, TSPyV is associated with Trichodysplasia spinulosa, a rare skin disease only seen in immunocompromised patients. The virus causes hyperproliferation and enlargement of hair follicles by modulating PP2A protein phosphatase signaling pathways. TSPyV was the eighth human polyomavirus to be discovered, and one of four associated with human disease, out of 13 human polyomaviruses known as of the 2015 update to polyomavirus taxonomy released by the International Committee on Taxonomy of Viruses.

Topical steroid withdrawal, also known as red burning skin and steroid dermatitis, has been reported in users of topical steroids after they stop the use, following usually any more than 2 weeks in duration. Symptoms include redness of the skin, a burning sensation, and itchiness. This may then be followed by skin peeling.
Hamster polyomavirus is an unenveloped double-stranded DNA virus of the polyomavirus family whose natural host is the hamster. It was originally described in 1967 by Arnold Graffi as a cause of epithelioma in Syrian hamsters.
WU polyomavirus is a virus of the family Polyomaviridae. It was discovered in 2007 in samples of human respiratory secretions, originally from a child patient in Australia who presented with clinical signs of pneumonia and in whom other common respiratory viruses were not detected. Follow-up studies identified the presence of WU virus in respiratory secretion samples from patients in Australia and the United States, suggesting that, like other human polyomaviruses, WU virus is widely distributed.
KI polyomavirus is a virus of the family Polyomaviridae. It was discovered in 2007 in stored samples of human respiratory secretions collected by the Karolinska Institute, after which the virus is named.
Human polyomavirus 7 (HPyV7) is a virus of the polyomavirus family that infects human hosts. It was discovered in 2010 and is a common component of the skin flora in healthy adults. There is limited evidence from case reports linking the virus to a skin rash occurring in immunocompromised organ transplant recipients.
Human polyomavirus 6 (HPyV6) is a virus of the polyomavirus family that infects human hosts. It was discovered in 2010 and is a component of the skin flora in healthy adults.
Human polyomavirus 9 (HPyV9) is a virus of the polyomavirus family that infects human hosts. It was discovered in 2011 and is a component of the skin flora in healthy adults.
Sorex araneus polyomavirus 1, formerly known as Human polyomavirus 12 (HPyV12), is a virus of the polyomavirus family that was first identified in human hosts and also infects shrews. It was discovered and reported in 2013 after isolation from the organs of the gastrointestinal tract, particularly the liver. The virus was renamed to Sorex araneus polyomavirus 1 in 2018, after discovery of the same virus in shrews. Infecting multiple hosts is rare among mammalian polyomaviruses.
New Jersey polyomavirus is a virus of the polyomavirus family that infects human hosts. It was first identified in 2014 in a pancreatic transplant patient in New Jersey. It is the 13th and most recent human polyomavirus to be described.
The middle tumor antigen is a protein encoded in the genomes of some polyomaviruses, which are small double-stranded DNA viruses. MTag is expressed early in the infectious cycle along with two other related proteins, the small tumor antigen and large tumor antigen. MTag occurs only in a few known polyomaviruses, while STag and LTag are universal - it was first identified in mouse polyomavirus (MPyV), the first polyomavirus discovered, and also occurs in hamster polyomavirus. In MPyV, MTag is an efficient oncoprotein that can be sufficient to induce neoplastic transformation in some cells.
Cutaneous manifestations of COVID-19 are characteristic signs or symptoms of the Coronavirus disease 2019 that occur in the skin. The American Academy of Dermatology reports that skin lesions such as morbilliform, pernio, urticaria, macular erythema, vesicular purpura, papulosquamous purpura and retiform purpura are seen in people with COVID-19. Pernio-like lesions were more common in mild disease while retiform purpura was seen only in critically ill patients. The major dermatologic patterns identified in individuals with COVID-19 are urticarial rash, confluent erythematous/morbilliform rash, papulovesicular exanthem, chilbain-like acral pattern, livedo reticularis and purpuric “vasculitic” pattern. Chilblains and Multisystem inflammatory syndrome in children are also cutaneous manifestations of COVID-19.