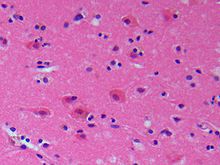
The cerebral cortex, also known as the cerebral mantle, is the outer layer of neural tissue of the cerebrum of the brain in humans and other mammals. It is the largest site of neural integration in the central nervous system. and plays a key role in attention, perception, awareness, thought, memory, language, and consciousness. The cerebral cortex is part of the brain responsible for cognition.

Colpocephaly is a cephalic disorder involving the disproportionate enlargement of the occipital horns of the lateral ventricles and is usually diagnosed early after birth due to seizures. It is a nonspecific finding and is associated with multiple neurological syndromes, including agenesis of the corpus callosum, Chiari malformation, lissencephaly, and microcephaly. Although the exact cause of colpocephaly is not known yet, it is commonly believed to occur as a result of neuronal migration disorders during early brain development, intrauterine disturbances, perinatal injuries, and other central nervous system disorders. Individuals with colpocephaly have various degrees of motor disabilities, visual defects, spasticity, and moderate to severe intellectual disability. No specific treatment for colpocephaly exists, but patients may undergo certain treatments to improve their motor function or intellectual disability.

The parietal lobe is one of the four major lobes of the cerebral cortex in the brain of mammals. The parietal lobe is positioned above the temporal lobe and behind the frontal lobe and central sulcus.

The frontal lobe is the largest of the four major lobes of the brain in mammals, and is located at the front of each cerebral hemisphere. It is parted from the parietal lobe by a groove between tissues called the central sulcus and from the temporal lobe by a deeper groove called the lateral sulcus. The most anterior rounded part of the frontal lobe is known as the frontal pole, one of the three poles of the cerebrum.

The occipital lobe is one of the four major lobes of the cerebral cortex in the brain of mammals. The name derives from its position at the back of the head, from the Latin ob, 'behind', and caput, 'head'.

The brain is the central organ of the human nervous system, and with the spinal cord makes up the central nervous system. The brain consists of the cerebrum, the brainstem and the cerebellum. It controls most of the activities of the body, processing, integrating, and coordinating the information it receives from the sense organs, and making decisions as to the instructions sent to the rest of the body. The brain is contained in, and protected by, the skull bones of the head.

Polymicrogyria (PMG) is a condition that affects the development of the human brain by multiple small gyri (microgyri) creating excessive folding of the brain leading to an abnormally thick cortex. This abnormality can affect either one region of the brain or multiple regions.
Bilateral frontoparietal polymicrogyria is a genetic disorder with autosomal recessive inheritance that causes a cortical malformation. Our brain has folds in the cortex to increase surface area called gyri and patients with polymicrogyria have an increase number of folds and smaller folds than usual. Polymicrogyria is defined as a cerebral malformation of cortical development in which the normal gyral pattern of the surface of the brain is replaced by an excessive number of small, fused gyri separated by shallow sulci and abnormal cortical lamination. From ongoing research, mutation in GPR56, a member of the adhesion G protein-coupled receptor (GPCR) family, results in BFPP. These mutations are located in different regions of the protein without any evidence of a relationship between the position of the mutation and phenotypic severity. It is also found that GPR56 plays a role in cortical pattering.

In neuroanatomy, a gyrus is a ridge on the cerebral cortex. It is generally surrounded by one or more sulci. Gyri and sulci create the folded appearance of the brain in humans and other mammals.

The lobes of the brain are the major identifiable zones of the human cerebral cortex, and they comprise the surface of each hemisphere of the cerebrum. The two hemispheres are roughly symmetrical in structure, and are connected by the corpus callosum. They traditionally have been divided into four lobes, but are today considered as having six lobes each. The lobes are large areas that are anatomically distinguishable, and are also functionally distinct to some degree. Each lobe of the brain has numerous ridges, or gyri, and furrows, the sulci that constitute further subzones of the cortex. The expression "lobes of the brain" usually refers only to those of the cerebrum, not to the distinct areas of the cerebellum.

Periventricular leukomalacia (PVL) is a form of white-matter brain injury, characterized by the necrosis of white matter near the lateral ventricles. It can affect newborns and fetuses; premature infants are at the greatest risk of neonatal encephalopathy which may lead to this condition. Affected individuals generally exhibit motor control problems or other developmental delays, and they often develop cerebral palsy or epilepsy later in life. The white matter in preterm born children is particularly vulnerable during the third trimester of pregnancy when white matter developing takes place and the myelination process starts around 30 weeks of gestational age.
Pachygyria is a congenital malformation of the cerebral hemisphere. It results in unusually thick convolutions of the cerebral cortex. Typically, children have developmental delay and seizures, the onset and severity depending on the severity of the cortical malformation. Infantile spasms are common in affected children, as is intractable epilepsy.

The inferior temporal gyrus is one of three gyri of the temporal lobe and is located below the middle temporal gyrus, connected behind with the inferior occipital gyrus; it also extends around the infero-lateral border on to the inferior surface of the temporal lobe, where it is limited by the inferior sulcus. This region is one of the higher levels of the ventral stream of visual processing, associated with the representation of objects, places, faces, and colors. It may also be involved in face perception, and in the recognition of numbers and words.

Foix–Chavany–Marie syndrome (FCMS), also known as bilateral opercular syndrome, is a neuropathological disorder characterized by paralysis of the facial, tongue, pharynx, and masticatory muscles of the mouth that aid in chewing. The disorder is primarily caused by thrombotic and embolic strokes, which cause a deficiency of oxygen in the brain. As a result, bilateral lesions may form in the junctions between the frontal lobe and temporal lobe, the parietal lobe and cortical lobe, or the subcortical region of the brain. FCMS may also arise from defects existing at birth that may be inherited or nonhereditary. Symptoms of FCMS can be present in a person of any age and it is diagnosed using automatic-voluntary dissociation assessment, psycholinguistic testing, neuropsychological testing, and brain scanning. Treatment for FCMS depends on the onset, as well as on the severity of symptoms, and it involves a multidisciplinary approach.

The superior longitudinal fasciculus (SLF) is an association tract in the brain that is composed of three separate components. It is present in both hemispheres and can be found lateral to the centrum semiovale and connects the frontal, occipital, parietal, and temporal lobes. This bundle of tracts (fasciculus) passes from the frontal lobe through the operculum to the posterior end of the lateral sulcus where they either radiate to and synapse on neurons in the occipital lobe, or turn downward and forward around the putamen and then radiate to and synapse on neurons in anterior portions of the temporal lobe.

The posterior parietal cortex plays an important role in planned movements, spatial reasoning, and attention.
Gyrification is the process of forming the characteristic folds of the cerebral cortex.
Form perception is the recognition of visual elements of objects, specifically those to do with shapes, patterns and previously identified important characteristics. An object is perceived by the retina as a two-dimensional image, but the image can vary for the same object in terms of the context with which it is viewed, the apparent size of the object, the angle from which it is viewed, how illuminated it is, as well as where it resides in the field of vision. Despite the fact that each instance of observing an object leads to a unique retinal response pattern, the visual processing in the brain is capable of recognizing these experiences as analogous, allowing invariant object recognition. Visual processing occurs in a hierarchy with the lowest levels recognizing lines and contours, and slightly higher levels performing tasks such as completing boundaries and recognizing contour combinations. The highest levels integrate the perceived information to recognize an entire object. Essentially object recognition is the ability to assign labels to objects in order to categorize and identify them, thus distinguishing one object from another. During visual processing information is not created, but rather reformatted in a way that draws out the most detailed information of the stimulus.
Pathoclisis is the theory that certain specialized parts of the brain are the first to be damaged in the case of disease, lack of oxygen, or malnutrition. The selective vulnerability of certain neurons can then lead to the expression of pathology. The APA dictionary of psychology defines pathoclisis as “sensitivity to particular toxins, or the tendency of particular toxins to target certain organs or systems of organ.”

Occipital epilepsy is a neurological disorder that arises from excessive neural activity in the occipital lobe of the brain that may or may not be symptomatic. Occipital lobe epilepsy is fairly rare, and may sometimes be misdiagnosed as migraine when symptomatic. Epileptic seizures are the result of synchronized neural activity that is excessive, and may stem from a failure of inhibitory neurons to regulate properly.