Chorioretinitis is an inflammation of the choroid and retina of the eye. It is a form of posterior uveitis. Inflammation of these layers can lead to vision-threatening complications. If only the choroid is inflamed, not the retina, the condition is termed choroiditis. The ophthalmologist's goal in treating these potentially blinding conditions is to eliminate the inflammation and minimize the potential risk of therapy to the patient.
Daclizumab is a therapeutic humanized monoclonal antibody which was used for the treatment of adults with relapsing forms of multiple sclerosis (MS). Daclizumab works by binding to CD25, the alpha subunit of the IL-2 receptor of T-cells.
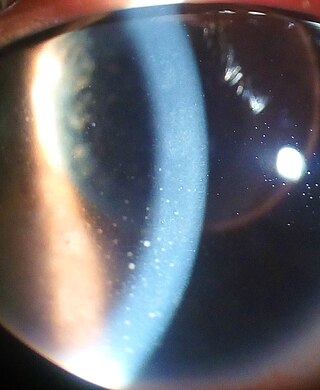
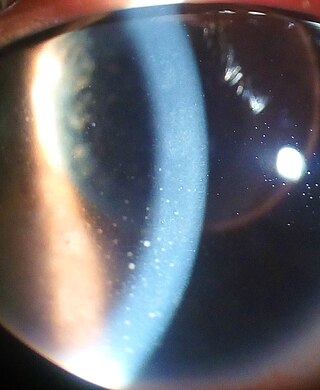
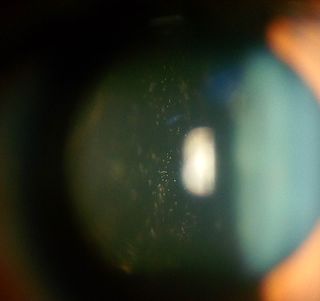
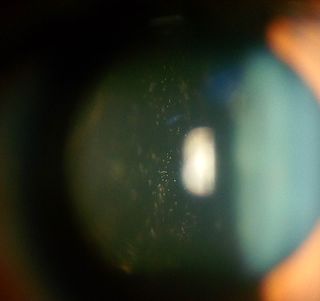
Uveitis is inflammation of the uvea, the pigmented layer of the eye between the inner retina and the outer fibrous layer composed of the sclera and cornea. The uvea consists of the middle layer of pigmented vascular structures of the eye and includes the iris, ciliary body, and choroid. Uveitis is described anatomically, by the part of the eye affected, as anterior, intermediate or posterior, or panuveitic if all parts are involved. Anterior uveitis (iridocyclitis) is the most common, with the incidence of uveitis overall affecting approximately 1:4500, most commonly those between the ages of 20-60. Symptoms include eye pain, eye redness, floaters and blurred vision, and ophthalmic examination may show dilated ciliary blood vessels and the presence of cells in the anterior chamber. Uveitis may arise spontaneously, have a genetic component, or be associated with an autoimmune disease or infection. While the eye is a relatively protected environment, its immune mechanisms may be overcome resulting in inflammation and tissue destruction associated with T-cell activation.

Central serous chorioretinopathy, also known as central serous retinopathy (CSR), is an eye disease that causes visual impairment, often temporary, usually in one eye. When the disorder is active it is characterized by leakage of fluid under the retina that has a propensity to accumulate under the central macula. This results in blurred or distorted vision (metamorphopsia). A blurred or gray spot in the central visual field is common when the retina is detached. Reduced visual acuity may persist after the fluid has disappeared.

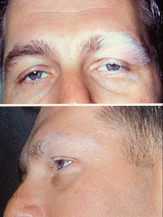
Choroideremia is a rare, X-linked recessive form of hereditary retinal degeneration that affects roughly 1 in 50,000 males. The disease causes a gradual loss of vision, starting with childhood night blindness, followed by peripheral vision loss and progressing to loss of central vision later in life. Progression continues throughout the individual's life, but both the rate of change and the degree of visual loss are variable among those affected, even within the same family.
Intermediate uveitis is a form of uveitis localized to the vitreous and peripheral retina. Primary sites of inflammation include the vitreous of which other such entities as pars planitis, posterior cyclitis, and hyalitis are encompassed. Intermediate uveitis may either be an isolated eye disease or associated with the development of a systemic disease such as multiple sclerosis or sarcoidosis. As such, intermediate uveitis may be the first expression of a systemic condition. Infectious causes of intermediate uveitis include Epstein–Barr virus infection, Lyme disease, HTLV-1 virus infection, cat scratch disease, and hepatitis C.

HLA-DR1 (DR1) is a HLA-DR serotype that recognizes the DRB1*01 gene products. It has been observed to be common among centenarians.

Acute posterior multifocal placoid pigment epitheliopathy (APMPPE) is an acquired inflammatory uveitis that belongs to the heterogenous group of white dot syndromes in which light-coloured (yellowish-white) lesions begin to form in the macular area of the retina. Early in the course of the disease, the lesions cause acute and marked vision loss that ranges from mild to severe but is usually transient in nature. APMPPE is classified as an inflammatory disorder that is usually bilateral and acute in onset but self-limiting. The lesions leave behind some pigmentation, but visual acuity eventually improves even without any treatment.

Type 1 tumor necrosis factor receptor shedding aminopeptidase regulator, also known as endoplasmic reticulum aminopeptidase 1 (ARTS-1), is a protein which in humans is encoded by the ARTS-1 gene.
Acute retinal necrosis (ARN) is a medical inflammatory condition of the eye. The condition presents itself as a necrotizing retinitis. The inflammation onset is due to certain herpes viruses, varicella zoster virus (VZV), herpes simplex virus (HSV-1 and HSV-2) and Epstein–Barr virus (EBV).

HLA-B51 (B51) is an HLA-B serotype. The serotype identifies the more common HLA-B*51 gene products.
White dot syndromes are inflammatory diseases characterized by the presence of white dots on the fundus, the interior surface of the eye. The majority of individuals affected with white dot syndromes are younger than fifty years of age. Some symptoms include blurred vision and visual field loss. There are many theories for the etiology of white dot syndromes including infectious, viral, genetics and autoimmune.
Douglas Jabs is an American ophthalmologist and an expert in clinical research in the fields of ophthalmology and uveitis.

Retinal vasculitis is inflammation of the vascular branches of the retinal artery, caused either by primary ocular disease processes, or as a specific presentation of any systemic form of vasculitis such as Behçet's disease, sarcoidosis, multiple sclerosis, or any form of systemic necrotizing vasculitis such as temporal arteritis, polyarteritis nodosa, and granulomatosis with polyangiitis, or due to lupus erythematosus, or rheumatoid arthritis. Eales disease, pars planitis, birdshot retinochoroidopathy, and Fuchs heterochromic iridocyclitis (FHI) can also cause retinal vasculitis. Infectious pathogens such as Mycobacterium tuberculosis, visceral larva migrans can also cause retinal vasculitis. Drug-induced vasculitis may involve retina as well, as seen in methamphetamine induced vasculitis.

Behçet's disease (BD) is a type of inflammatory disorder which affects multiple parts of the body. The most common symptoms include painful sores on the mucous membranes of the mouth and other parts of the body, inflammation of parts of the eye, and arthritis. The sores can last from a few days, up to a week or more. Less commonly there may be inflammation of the brain or spinal cord, blood clots, aneurysms, or blindness. Often, the symptoms come and go.

Toxoplasma chorioretinitis, more simply known as ocular toxoplasmosis, is possibly the most common cause of infections in the back of the eye worldwide. The causitive agent is Toxoplasma gondii, and in the United States, most cases are acquired congenitally. The most common symptom is decreased visual acuity in one eye. The diagnosis is made by examination of the eye, using ophthalmoscopy. Sometimes serologic testing is used to rule out the disease, but due to high rates of false positives, serologies are not diagnostic of toxoplasmic retinitis.
Multiple evanescent white dot syndrome (MEWDS) is an uncommon inflammatory condition of the retina that typically affects otherwise healthy young females in the second to fourth decades of life.
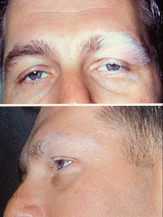
Vogt–Koyanagi–Harada disease (VKH) is a multisystem disease of presumed autoimmune cause that affects melanin-pigmented tissues. The most significant manifestation is bilateral, diffuse uveitis, which affects the eyes. VKH may variably also involve the inner ear, with effects on hearing, the skin, and the meninges of the central nervous system.
Occult macular dystrophy (OMD) is a rare inherited degradation of the retina, characterized by progressive loss of function in the most sensitive part of the central retina (macula), the location of the highest concentration of light-sensitive cells (photoreceptors) but presenting no visible abnormality. "Occult" refers to the degradation in the fundus being difficult to discern. The disorder is called "dystrophy" instead of "degradation" to distinguish its genetic origin from other causes, such as age. OMD was first reported by Y. Miyake et al. in 1989.

Uveitic glaucoma is most commonly a progression stage of noninfectious anterior uveitis or iritis.