Idiopathic intracranial hypertension (IIH), previously known as pseudotumor cerebri and benign intracranial hypertension, is a condition characterized by increased intracranial pressure without a detectable cause. The main symptoms are headache, vision problems, ringing in the ears, and shoulder pain. Complications may include vision loss.

Cranial nerves are the nerves that emerge directly from the brain, of which there are conventionally considered twelve pairs. Cranial nerves relay information between the brain and parts of the body, primarily to and from regions of the head and neck, including the special senses of vision, taste, smell, and hearing.

Anosmia, also known as smell blindness, is the loss of the ability to detect one or more smells. Anosmia may be temporary or permanent. It differs from hyposmia, which is a decreased sensitivity to some or all smells.

Papilledema or papilloedema is optic disc swelling that is caused by increased intracranial pressure due to any cause. The swelling is usually bilateral and can occur over a period of hours to weeks. Unilateral presentation is extremely rare.

Craniosynostosis is a condition in which one or more of the fibrous sutures in a young infant's skull prematurely fuses by turning into bone (ossification), thereby changing the growth pattern of the skull. Because the skull cannot expand perpendicular to the fused suture, it compensates by growing more in the direction parallel to the closed sutures. Sometimes the resulting growth pattern provides the necessary space for the growing brain, but results in an abnormal head shape and abnormal facial features. In cases in which the compensation does not effectively provide enough space for the growing brain, craniosynostosis results in increased intracranial pressure leading possibly to visual impairment, sleeping impairment, eating difficulties, or an impairment of mental development combined with a significant reduction in IQ.

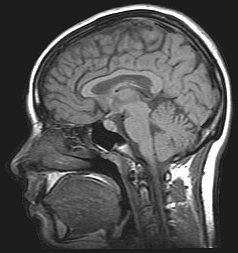
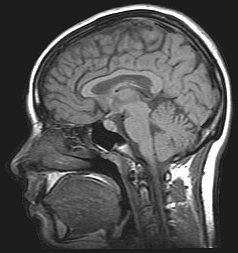
Brain herniation is a potentially deadly side effect of very high pressure within the skull that occurs when a part of the brain is squeezed across structures within the skull. The brain can shift across such structures as the falx cerebri, the tentorium cerebelli, and even through the foramen magnum. Herniation can be caused by a number of factors that cause a mass effect and increase intracranial pressure (ICP): these include traumatic brain injury, intracranial hemorrhage, or brain tumor.
The posterior cerebral artery (PCA) is one of a pair of cerebral arteries that supply oxygenated blood to the occipital lobe, part of the back of the human brain. The two arteries originate from the distal end of the basilar artery, where it bifurcates into the left and right posterior cerebral arteries. These anastomose with the middle cerebral arteries and internal carotid arteries via the posterior communicating arteries.

Optic nerve sheath meningiomas (ONSM) are rare benign tumors of the optic nerve. 60–70% of cases occur in middle age females, and is more common in older adults. It is also seen in children, but this is rare. The tumors grow from cells that surround the optic nerve, and as the tumor grows, it compresses the optic nerve. This causes loss of vision in the affected eye. Rarely, it may affect both eyes at the same time.

Sixth nerve palsy, or abducens nerve palsy, is a disorder associated with dysfunction of cranial nerve VI, which is responsible for causing contraction of the lateral rectus muscle to abduct the eye. The inability of an eye to turn outward, results in a convergent strabismus or esotropia of which the primary symptom is diplopia in which the two images appear side-by-side. Thus, the diplopia is horizontal and worse in the distance. Diplopia is also increased on looking to the affected side and is partly caused by overaction of the medial rectus on the unaffected side as it tries to provide the extra innervation to the affected lateral rectus. These two muscles are synergists or "yoke muscles" as both attempt to move the eye over to the left or right. The condition is commonly unilateral but can also occur bilaterally.

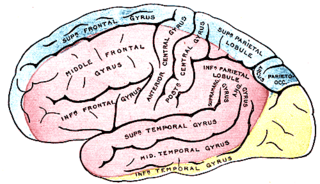
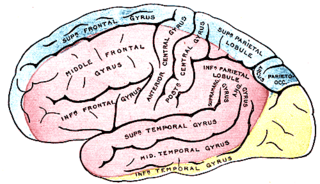
Frontal lobe disorder, also frontal lobe syndrome, is an impairment of the frontal lobe of the brain due to disease or frontal lobe injury. The frontal lobe plays a key role in executive functions such as motivation, planning, social behaviour, and speech production. Frontal lobe syndrome can be caused by a range of conditions including head trauma, tumours, neurodegenerative diseases, neurodevelopmental disorders, neurosurgery and cerebrovascular disease. Frontal lobe impairment can be detected by recognition of typical signs and symptoms, use of simple screening tests, and specialist neurological testing.

A sphenoid wing meningioma is a benign brain tumor near the sphenoid bone.

The olfactory peduncle is a bilateral bundle of afferent nerve fibers from the mitral and tufted cells of the olfactory bulb that connects to several target regions in the brain, including the piriform cortex, amygdala, and entorhinal cortex. It is a narrow white band, triangular on coronal section, the apex being directed upward.
Optic neuropathy is damage to the optic nerve from any cause. The optic nerve is a bundle of millions of fibers in the retina that sends visual signals to the brain.

Optic disc drusen (ODD) are globules of mucoproteins and mucopolysaccharides that progressively calcify in the optic disc. They are thought to be the remnants of the axonal transport system of degenerated retinal ganglion cells. ODD have also been referred to as congenitally elevated or anomalous discs, pseudopapilledema, pseudoneuritis, buried disc drusen, and disc hyaline bodies.
Focal neurologic signs also known as focal neurological deficits or focal CNS signs are impairments of nerve, spinal cord, or brain function that affects a specific region of the body, e.g. weakness in the left arm, the right leg, paresis, or plegia.

Chiasmal syndrome is the set of signs and symptoms that are associated with lesions of the optic chiasm, manifesting as various impairments of the affected's visual field according to the location of the lesion along the optic nerve. Pituitary adenomas are the most common cause; however, chiasmal syndrome may be caused by cancer, or associated with other medical conditions such as multiple sclerosis and neurofibromatosis.
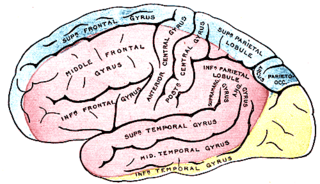
Anterior cerebral artery syndrome is a condition whereby the blood supply from the anterior cerebral artery (ACA) is restricted, leading to a reduction of the function of the portions of the brain supplied by that vessel: the medial aspects of the frontal and parietal lobes, basal ganglia, anterior fornix and anterior corpus callosum.
The cerebellopontine angle syndrome is a distinct neurological syndrome of deficits that can arise due to the closeness of the cerebellopontine angle to specific cranial nerves. Indications include unilateral hearing loss (85%), speech impediments, disequilibrium, tremors or other loss of motor control. The cerebellopontine angle cistern is a subarachnoid cistern formed by the cerebellopontine angle that lies between the cerebellum and the pons. It is filled with cerebrospinal fluid and is a common site for the growth of acoustic neuromas or schwannomas.
Kernohan's notch is a cerebral peduncle indentation associated with some forms of transtentorial herniation. It is a secondary condition caused by a primary injury on the opposite hemisphere of the brain. Kernohan's notch is an ipsilateral condition, in that a left-sided primary lesion evokes motor impairment in the left side of the body and a right-sided primary injury evokes motor impairment in the right side of the body. The seriousness of Kernohan's notch varies depending on the primary problem causing it, which may range from benign brain tumors to advanced subdural hematoma.

The visual pathway consists of structures that carry visual information from the retina to the brain. Lesions in that pathway cause a variety of visual field defects. In the visual system of human eye, the visual information processed by retinal photoreceptor cells travel in the following way:
Retina→Optic nerve→Optic chiasma →Optic tract→Lateral geniculate body→Optic radiation→Primary visual cortex