The choroid, also known as the choroidea or choroid coat, is a part of the uvea, the vascular layer of the eye. It contains connective tissues, and lies between the retina and the sclera. The human choroid is thickest at the far extreme rear of the eye, while in the outlying areas it narrows to 0.1 mm. The choroid provides oxygen and nourishment to the outer layers of the retina. Along with the ciliary body and iris, the choroid forms the uveal tract.

Amaurosis fugax is a painless temporary loss of vision in one or both eyes.

Fluorescein angiography (FA), fluorescent angiography (FAG), or fundus fluorescein angiography (FFA) is a technique for examining the circulation of the retina and choroid using a fluorescent dye and a specialized camera. Sodium fluorescein is added into the systemic circulation, the retina is illuminated with blue light at a wavelength of 490 nanometers, and an angiogram is obtained by photographing the fluorescent green light that is emitted by the dye. The fluorescein is administered intravenously in intravenous fluorescein angiography (IVFA) and orally in oral fluorescein angiography (OFA). The test is a dye tracing method.

The optic disc or optic nerve head is the point of exit for ganglion cell axons leaving the eye. Because there are no rods or cones overlying the optic disc, it corresponds to a small blind spot in each eye.
Anterior ischemic optic neuropathy (AION) is a medical condition involving loss of vision caused by damage to the optic nerve as a result of insufficient blood supply (ischemia). This form of ischemic optic neuropathy is generally categorized as two types: arteritic AION, in which the loss of vision is the result of an inflammatory disease of arteries in the head called temporal arteritis, and non-arteritic AION, which is due to non-inflammatory disease of small blood vessels.
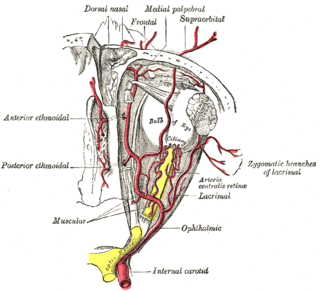
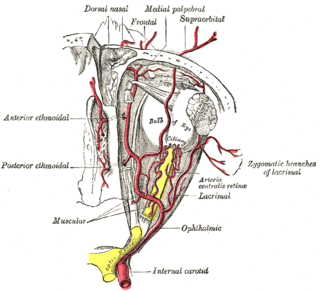
The ophthalmic artery (OA) is an artery of the head. It is the first branch of the internal carotid artery distal to the cavernous sinus. Branches of the ophthalmic artery supply all the structures in the orbit around the eye, as well as some structures in the nose, face, and meninges. Occlusion of the ophthalmic artery or its branches can produce sight-threatening conditions.

The central retinal artery branches off the ophthalmic artery, running inferior to the optic nerve within its dural sheath to the eyeball.

A Hollenhorst plaque is a cholesterol embolus that is seen in a blood vessel of the retina. It is usually found when a physician performs ophthalmoscopy, during which a plaque will appear as a small, bright crystal that is refractile and yellow. This is a medical exam finding, and is not a medical condition, though it may be related to cardiovascular conditions such as atherosclerosis of the internal carotid artery. It was first described by American ophthalmologist Robert Hollenhorst in 1961.
Eales disease is a type of obliterative vasculopathy, also known as angiopathia retinae juvenilis, periphlebitis retinae or primary perivasculitis of the retina. It was first described by the British ophthalmologist Henry Eales (1852–1913) in 1880 and is a rare ocular disease characterized by inflammation and possible blockage of retinal blood vessels, abnormal growth of new blood vessels (neovascularization), and recurrent retinal and vitreal hemorrhages.
Ocular ischemic syndrome is the constellation of ocular signs and symptoms secondary to severe, chronic arterial hypoperfusion to the eye. Amaurosis fugax is a form of acute vision loss caused by reduced blood flow to the eye; it may be a warning sign of an impending stroke, as both stroke and retinal artery occlusion can be caused by thromboembolism due to atherosclerosis elsewhere in the body. Consequently, those with transient blurring of vision are advised to urgently seek medical attention for a thorough evaluation of the carotid artery. Anterior segment ischemic syndrome is a similar ischemic condition of anterior segment usually seen in post-surgical cases. Retinal artery occlusion leads to rapid death of retinal cells, thereby resulting in severe loss of vision.

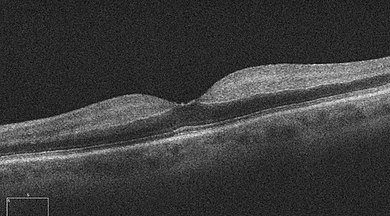
Optic disc drusen (ODD) are globules of mucoproteins and mucopolysaccharides that progressively calcify in the optic disc. They are thought to be the remnants of the axonal transport system of degenerated retinal ganglion cells. ODD have also been referred to as congenitally elevated or anomalous discs, pseudopapilledema, pseudoneuritis, buried disc drusen, and disc hyaline bodies.
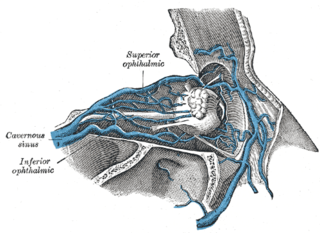
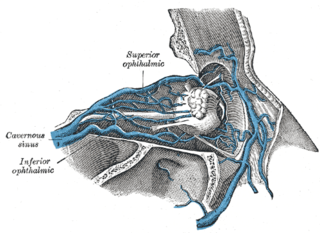
The central retinal vein is a vein that drains the retina of the eye. It travels backwards through the centre of the optic nerve accompanied by the central retinal artery before exiting the optic nerve together with the central retinal artery to drain into either the superior ophthalmic vein or the cavernous sinus.

Fundus photography involves photographing the rear of an eye, also known as the fundus. Specialized fundus cameras consisting of an intricate microscope attached to a flash enabled camera are used in fundus photography. The main structures that can be visualized on a fundus photo are the central and peripheral retina, optic disc and macula. Fundus photography can be performed with colored filters, or with specialized dyes including fluorescein and indocyanine green.

Central retinal vein occlusion, also CRVO, is when the central retinal vein becomes occluded, usually through thrombosis. The central retinal vein is the venous equivalent of the central retinal artery and both may become occluded. Since the central retinal artery and vein are the sole source of blood supply and drainage for the retina, such occlusion can lead to severe damage to the retina and blindness, due to ischemia and edema (swelling).

Bonnet–Dechaume–Blanc syndrome, also known as Wyburn-Mason syndrome, is a rare congenital disorder characterized by arteriovenous malformations of the brain, retina or facial nevi. The syndrome has a number of possible symptoms and can, more rarely, affect the skin, bones, kidneys, muscles, and gastrointestinal tract. When the syndrome affects the brain, people can experience severe headaches, seizures, acute stroke, meningism, and progressive neurological deficits due to acute or chronic ischaemia caused by arteriovenous shunting.
Sohan Singh Hayreh was an ophthalmologist, clinical scientist, and professor emeritus of ophthalmology at the University of Iowa. As one of the pioneers in the field of fluorescein angiography, he was generally acknowledged to be a leading authority in vascular diseases of the eye and the optic nerve. For over 60 years, Hayreh was actively involved in basic, experimental, and clinical research in ophthalmology, publishing over 400 original peer-reviewed articles in various international ophthalmic journals, six classical monographs and books in his field of research, and more than 50 chapters in ophthalmic books. He made many seminal observations dealing with the ocular circulation in health and disease, the optic disc and the optic nerve, retinal and choroidal vascular disorders, glaucomatous optic neuropathy, fundus changes in malignant arterial hypertension, ocular neovascularization, rheumatologic disorders of the eye, and nocturnal arterial hypotension. He was an elected fellow of the National Academy of Medical Sciences.

Branch retinal artery occlusion (BRAO) is a rare retinal vascular disorder in which one of the branches of the central retinal artery is obstructed.

Branch retinal vein occlusion is a common retinal vascular disease of the elderly. It is caused by the occlusion of one of the branches of central retinal vein.
Sickle cell retinopathy can be defined as retinal changes due to blood vessel damage in the eye of a person with a background of sickle cell disease. It can likely progress to loss of vision in late stages due to vitreous hemorrhage or retinal detachment. Sickle cell disease is a structural red blood cell disorder leading to consequences in multiple systems. It is characterized by chronic red blood cell destruction, vascular injury, and tissue ischemia causing damage to the brain, eyes, heart, lungs, kidneys, spleen, and musculoskeletal system.
Drug abuse retinopathy is damage to the retina of the eyes caused by chronic drug abuse. Types of retinopathy caused by drug abuse include maculopathy, Saturday night retinopathy, and talc retinopathy. Common symptoms include temporary and permanent vision loss, blurred vision, and night blindness. Substances commonly associated with this condition include poppers, heroin, cocaine, methamphetamine, tobacco, and alcohol.