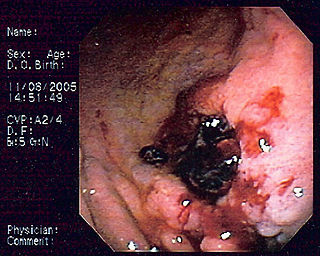
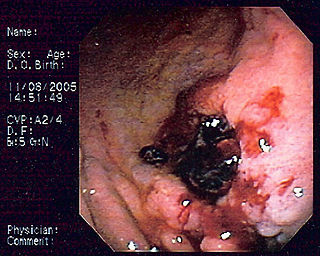
Peptic ulcer disease is a break in the inner lining of the stomach, the first part of the small intestine, or sometimes the lower esophagus. An ulcer in the stomach is called a gastric ulcer, while one in the first part of the intestines is a duodenal ulcer. The most common symptoms of a duodenal ulcer are waking at night with upper abdominal pain, and upper abdominal pain that improves with eating. With a gastric ulcer, the pain may worsen with eating. The pain is often described as a burning or dull ache. Other symptoms include belching, vomiting, weight loss, or poor appetite. About a third of older people with peptic ulcers have no symptoms. Complications may include bleeding, perforation, and blockage of the stomach. Bleeding occurs in as many as 15% of cases.

Helicobacter pylori, previously known as Campylobacter pylori, is a gram-negative, flagellated, helical bacterium. Mutants can have a rod or curved rod shape, and these are less effective. Its helical body is thought to have evolved in order to penetrate the mucous lining of the stomach, helped by its flagella, and thereby establish infection. The bacterium was first identified as the causal agent of gastric ulcers in 1983 by the Australian doctors Barry Marshall and Robin Warren.

Barry James Marshall is an Australian physician, Nobel Prize Laureate in Physiology or Medicine, Professor of Clinical Microbiology and Co-Director of the Marshall Centre at the University of Western Australia. Marshall and Robin Warren showed that the bacterium Helicobacter pylori plays a major role in causing many peptic ulcers, challenging decades of medical doctrine holding that ulcers were caused primarily by stress, spicy foods, and too much acid. This discovery has allowed for a breakthrough in understanding a causative link between Helicobacter pylori infection and stomach cancer.

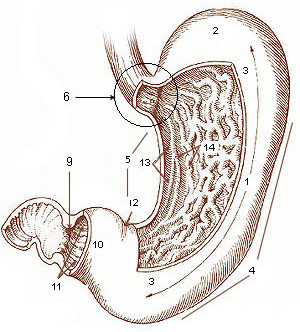
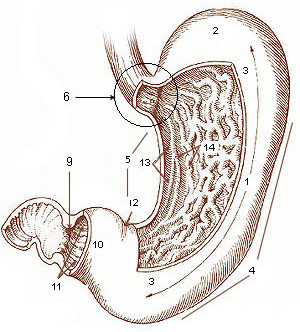
The pylorus, or pyloric part, connects the stomach to the duodenum. The pylorus is considered as having two parts, the pyloric antrum and the pyloric canal. The pyloric canal ends as the pyloric orifice, which marks the junction between the stomach and the duodenum. The orifice is surrounded by a sphincter, a band of muscle, called the pyloric sphincter. The word pylorus comes from Greek πυλωρός, via Latin. The word pylorus in Greek means "gatekeeper", related to "gate" and is thus linguistically related to the word "pylon".
Coffee ground vomitus refers to a particular appearance of vomit. Within organic heme molecules of red blood cells is the element iron, which oxidizes following exposure to gastric acid. This reaction causes the vomitus to look like ground coffee.

Esophagogastroduodenoscopy (EGD) or oesophagogastroduodenoscopy (OGD), also called by various other names, is a diagnostic endoscopic procedure that visualizes the upper part of the gastrointestinal tract down to the duodenum. It is considered a minimally invasive procedure since it does not require an incision into one of the major body cavities and does not require any significant recovery after the procedure. However, a sore throat is common.

Pyloric stenosis is a narrowing of the opening from the stomach to the first part of the small intestine. Symptoms include projectile vomiting without the presence of bile. This most often occurs after the baby is fed. The typical age that symptoms become obvious is two to twelve weeks old.
A gastrectomy is a partial or total surgical removal of the stomach.

A gastroenterostomy is the surgical creation of a connection between the stomach and the jejunum. The operation can sometimes be performed at the same time as a partial gastrectomy. Gastroenterostomy was in the past typically performed to treat peptic ulcers, but today it is usually carried out to enable food to pass directly to the middle section of the small intestine when it is necessary to bypass the first section because of duodenal damage. The procedure is still being used to treat gastroparesis that is refractory to other treatments, but it is now rarely used to treat peptic ulcers because most cases thereof are bacterial in nature and there are many new drugs available to treat the gastric reflux often experienced with peptic ulcer disease. Reported cure rates for H. pylori infection range from 70% to 90% after antibiotic treatment.

Gastrinomas are neuroendocrine tumors (NETs), usually located in the duodenum or pancreas, that secrete gastrin and cause a clinical syndrome known as Zollinger–Ellison syndrome (ZES). A large number of gastrinomas develop in the pancreas or duodenum, with near-equal frequency, and approximately 10% arise as primary neoplasms in lymph nodes of the pancreaticoduodenal region.
Primary gastric lymphoma is an uncommon condition, accounting for less than 15% of gastric malignancies and about 2% of all lymphomas. However, the stomach is a very common extranodal site for lymphomas. It is also the most common source of lymphomas in the gastrointestinal tract.

A vagotomy is a surgical procedure that involves removing part of the vagus nerve. It is performed in the abdomen.

This is a timeline of the events relating to the discovery that peptic ulcer disease and some cancers are caused by H. pylori. In 2005, Barry Marshall and Robin Warren were awarded the Nobel Prize in Physiology or Medicine for their discovery that peptic ulcer disease (PUD) was primarily caused by Helicobacter pylori, a bacterium with affinity for acidic environments, such as the stomach. As a result, PUD that is associated with H. pylori is currently treated with antibiotics used to eradicate the infection. For decades prior to their discovery, it was widely believed that PUD was caused by excess acid in the stomach. During this time, acid control was the primary method of treatment for PUD, to only partial success. Among other effects, it is now known that acid suppression alters the stomach milieu to make it less amenable to H. pylori infection.

A self-expandable metallic stent is a metallic tube, or stent that holds open a structure in the gastrointestinal tract to allow the passage of food, chyme, stool, or other secretions related to digestion. Surgeons insert SEMS by endoscopy, inserting a fibre optic camera—either through the mouth or colon—to reach an area of narrowing. As such, it is termed an endoprosthesis. SEMS can also be inserted using fluoroscopy where the surgeon uses an X-ray image to guide insertion, or as an adjunct to endoscopy.

Percutaneous transhepatic cholangiography, percutaneous hepatic cholangiogram (PTHC) is a radiological technique used to visualize the anatomy of the biliary tract. A contrast medium is injected into a bile duct in the liver, after which X-rays are taken. It allows access to the biliary tree in cases where endoscopic retrograde cholangiopancreatography has been unsuccessful. Initially reported in 1937, the procedure became popular in 1952.
A stress ulcer is a single or multiple mucosal defect usually caused by physiological stress which can become complicated by upper gastrointestinal bleeding. These ulcers can be caused by shock, sepsis, trauma or other conditions and are found in patients with chronic illnesses. These ulcers are a significant issue in patients in critical and intensive care.
Therapeutic endoscopy is the medical term for an endoscopic procedure during which treatment is carried out via the endoscope. This contrasts with diagnostic endoscopy, where the aim of the procedure is purely to visualize a part of the gastrointestinal, respiratory or urinary tract in order to aid diagnosis. In practice, a procedure which starts as a diagnostic endoscopy may become a therapeutic endoscopy depending on the findings, such as in cases of upper gastrointestinal bleeding, or the finding of polyps during colonoscopy.
A succussion splash, also known as a gastric splash, is a sloshing sound heard through a stethoscope during sudden movement of the patient on abdominal auscultation. It reflects the presence of gas and fluid in an obstructed organ, as in gastric outlet obstruction.

Pyloroplasty is a surgery performed to widen the opening at the lower part of the stomach, also known as the pylorus. When the pylorus thickens, it becomes difficult for food to pass through. The surgery is performed to widen the band of muscle known as the pyloric sphincter, a ring of smooth, muscular fibers that surrounds the pylorus and helps to regulate digestion and prevent reflux. The widening of the pyloric sphincter enables the contents of the stomach to pass into the first part of the small intestine known as the duodenum.

Antrectomy, also called distal gastrectomy, is a type of gastric resection surgery that involves the removal of the stomach antrum to treat gastric diseases causing the damage, bleeding, or blockage of the stomach. This is performed using either the Billroth I (BI) or Billroth II (BII) reconstruction method. Quite often, antrectomy is used alongside vagotomy to maximise its safety and effectiveness. Modern antrectomies typically have a high success rate and low mortality rate, but the exact numbers depend on the specific conditions being treated.