Problems
The neurocardiac axis is the link to many problems regarding the physiological functions of the body. This includes cardiac ischemia, stroke, epilepsy, and most importantly, heart arrhythmias and cardiac myopathies. Many of these problems are due to the imbalance of the nervous system, resulting in symptoms that affect both the heart and the brain. [6]
The connection between the cardiovascular and nervous system has brought up a concern in the training processes for medical students. Neurocardiology is the understanding that the body is interconnected and weave in and out of other systems. When training within one specialty, the doctors are more likely to associate patients' symptoms to their field. Without taking the integration into account, the doctor can consequently delay a correct diagnosis and treatment for the patient. [7] However, by specializing in a field, advancement in medicine continues as new findings come into perspective.[ citation needed ]
Stress

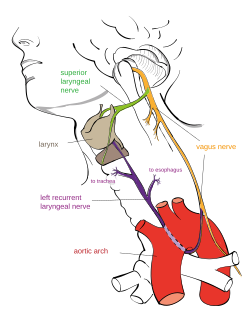
Cardiovascular systems are regulated by the autonomic nervous systems, which includes the sympathetic and parasympathetic nervous systems. A distinct balance between these two systems is crucial for the pathophysiology of cardiovascular disease. Chronic stress has been widely studied on its effects of the body resulting in an elevated heart rate (HR), reduced HR variability, elevated sympathetic tone, and intensified cardiovascular activity. Consequently, stress promotes an autonomic imbalance in favor of the sympathetic nervous system. The activation of the sympathetic nervous system contributes to endothelial dysfunction, hypertension, atherosclerosis, insulin resistance, and increased incidence of arrhythmias. [6] An imbalance in the autonomic nervous system has been documented in mood disorders; It is commonly regarded as a mediator between mood disorders and cardiovascular disorders.[ citation needed ]
The hypothalamus is the part of the brain that regulates function and responds to stress. When the brain perceives environmental danger, the amygdala fires a nerve impulse to the hypothalamus to initiate the body's fight-or-flight mode through the sympathetic nervous system. The stress response starts with the hypothalamus stimulating the pituitary gland, which releases the adrenocorticotropic hormone. This signals the release of cortisol, the stress hormone, initiating a multitude of physical effects on the body to aid in survival. The negative feedback loop is then needed to return the body to its resting state by signaling the parasympathetic nervous system. [8]
Prolonged stress leads to many hazards within the nervous system. Various hormones and glands become overworked, chemical waste is produced resulting in degeneration of nerve cells. The result of prolonged stress is the breakdown of the body and the nervous system. Stress alone does not produce potentially deadly arrhythmias in normal healthy hearts, however studies do appear to show that stress causes cardiac damage that may lead to arrhythmias.[ citation needed ]
Arrhythmias
In a study relating to relationship of neurocardiology of arrhythmias and sudden cardiac death, they hypothesized that the individual with a diseased heart has a greater likelihood of experiencing cardiac arrhythmias and sudden cardiac death when the neurocardiac axis is activated. [7] An arrhythmia is defined as any disturbance in the cardiac activation sequence or any deviation from accepted limits of rate or regularity of the normal impulse. The main types of arrhythmia leading to sudden cardiac death are tachyarrhythmias and bradyarrhythmias. Tachyarrhythmias are associated with ventricular fibrillation and ventricular tachycardia. Bradyarrhythmias are associated with complete atrioventricular blockage and sudden asystole. The underlying cause of sudden cardiac death is unclear, despite the understanding that heart disease causes arrhythmias, which in turn produce sudden cardiac death. [7] Lown describes the heart as the target, and the brain is called the trigger. Sudden cardiac death is triggered by an electrical accident, which can be treated with ventricular defibrillation. [9]
Stroke
Stroke activates the neurocardiac axis, producing arrhythmias, cardiac damage, and sudden death. In a recent study on patients with already diseased hearts and electrocardiographic abnormalities, there was evidence of lost hypothalamic-medullary integration at the midbrain. This resulted in the fact that overactivity in the parasympathetic nervous system may also cause sudden death with asystole after stroke. Catecholamine medications have been studied to mediate the effects of electrocardiographic changes and heart damage. [7]
Epilepsy
Sudden death from epilepsy is not very common, with a rate of approximately 2 in a thousand. The present understanding about how sudden cardiac death can result from epilepsy is that the brain is stimulating an arrhythmia. Recordings during seizures report that the onset of tachycardia just prior to the seizure is common, with both atrial and ventricular ectopy. [7] The sudden epileptic death may be a result of the sympathetic activation or autonomic imbalance of the nervous system as described earlier.[ citation needed ]
Emotions
The relationship between emotions and their effect on the destabilization of the heart continues to be a mystery. It is considered that both the spatial and temporal patterns of autonomic input to the heart play a key role in altered electrophysiological parameters. The body continually attempts to maintain homeostasis through the baroreflex. This balance in the autonomic neural input to the heart in response to the pressure and volume changes leads to alterations in the baroreceptors. [10]